2023-06-13 リンショーピング大学
◆この研究では、妊娠中における免疫細胞の変化を調査し、将来の治療戦略の発見につなげるために重要なメカニズムを明らかにしました。妊娠によってT細胞の遺伝子活性やエピジェネティックな変化が起こり、これらの変化が症状の改善と関連していることが示唆されました。また、妊娠ホルモンであるプロゲステロンが関与していることも明らかになり、将来の治療戦略におけるホルモンの役割が検証される予定です。
<関連情報>
- https://liu.se/en/news-item/why-women-with-multiple-sclerosis-get-better-when-pregnant
- https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-023-02781-2
多発性硬化症の女性および対照群における妊娠中および妊娠後のCD4+およびCD8+ T細胞における顕著なエピジェネティックおよびトランスクリプトーム変化 Prominent epigenetic and transcriptomic changes in CD4+ and CD8+ T cells during and after pregnancy in women with multiple sclerosis and controls
Alberto Zenere,Sandra Hellberg,Georgia Papapavlou Lingehed,Maria Svenvik,Johan Mellergård,Charlotte Dahle,Magnus Vrethem,Johanna Raffetseder,Mohsen Khademi,Tomas Olsson,Marie Blomberg,Maria C. Jenmalm,Claudio Altafini,Mika Gustafsson & Jan Ernerudh
Journal of Neuroinflammation Published:27 April 2023
DOI:https://doi.org/10.1186/s12974-023-02781-2
Abstract
Background
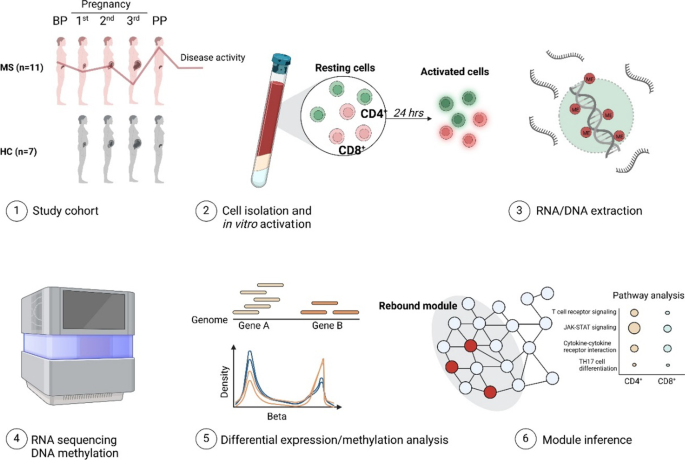
Multiple sclerosis (MS) is a neuroinflammatory disease in which pregnancy leads to a temporary amelioration in disease activity as indicated by the profound decrease in relapses rate during the 3rd trimester of pregnancy. CD4+ and CD8+ T cells are implicated in MS pathogenesis as being key regulators of inflammation and brain lesion formation. Although Tcells are prime candidates for the pregnancy-associated improvement of MS, the precise mechanisms are yet unclear, and in particular, a deep characterization of the epigenetic and transcriptomic events that occur in peripheral T cells during pregnancy in MS is lacking.
Methods
Women with MS and healthy controls were longitudinally sampled before, during (1st, 2nd and 3rd trimesters) and after pregnancy. DNA methylation array and RNA sequencing were performed on paired CD4+ and CD8+ T cells samples. Differential analysis and network-based approaches were used to analyze the global dynamics of epigenetic and transcriptomic changes.
Results
Both DNA methylation and RNA sequencing revealed a prominent regulation, mostly peaking in the 3rd trimester and reversing post-partum, thus mirroring the clinical course with improvement followed by a worsening in disease activity. This rebound pattern was found to represent a general adaptation of the maternal immune system, with only minor differences between MS and controls. By using a network-based approach, we highlighted several genes at the core of this pregnancy-induced regulation, which were found to be enriched for genes and pathways previously reported to be involved in MS. Moreover, these pathways were enriched for in vitro stimulated genes and pregnancy hormones targets.
Conclusion
This study represents, to our knowledge, the first in-depth investigation of the methylation and expression changes in peripheral CD4+ and CD8+ T cells during pregnancy in MS. Our findings indicate that pregnancy induces profound changes in peripheral T cells, in both MS and healthy controls, which are associated with the modulation of inflammation and MS activity.