2025-04-17 バージニア工科大学(VirginiaTech)
<関連情報>
- https://news.vt.edu/articles/2025/04/research-fralinbiomed-electrocancer-031025.html
- https://link.springer.com/article/10.1007/s10439-024-03674-y
4T1マウスモデルにおける亜切除的高周波非可逆エレクトロポレーション療法に伴う一過性のリンパ管リモデリング Transient Lymphatic Remodeling Follows Sub-Ablative High-Frequency Irreversible Electroporation Therapy in a 4T1 Murine Model
Savieay Esparza,Edward Jacobs,Jennifer H. Hammel,Sharon K. Michelhaugh,Nastaran Alinezhadbalalami,Margaret Nagai-Singer,Khan Mohammad Imran,Rafael V. Davalos,Irving C. Allen,Scott S. Verbridge & Jennifer M. Munson
Annals of Biomedical Engineering Published:25 February 2025
DOI:https://doi.org/10.1007/s10439-024-03674-y
Abstract
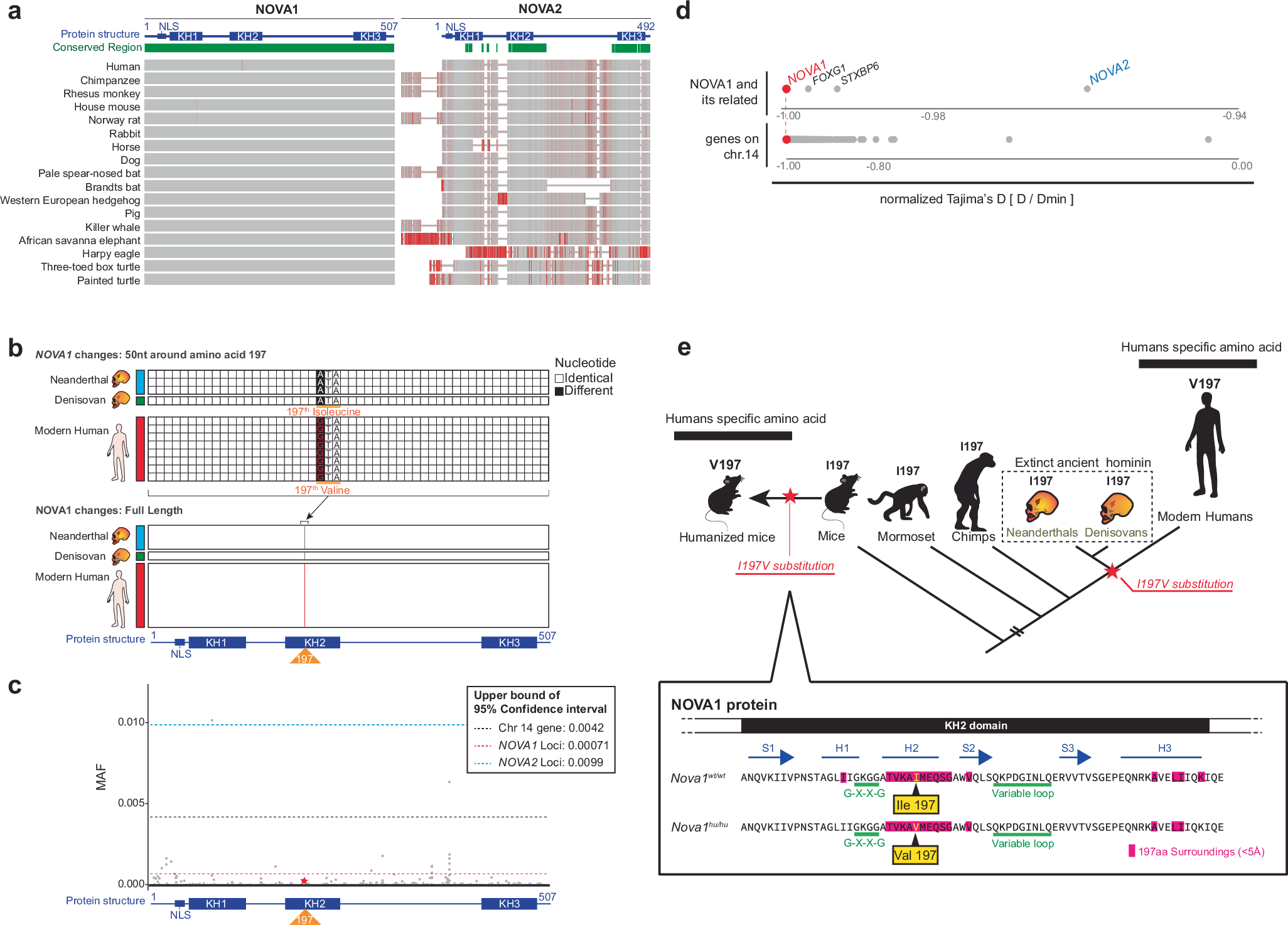
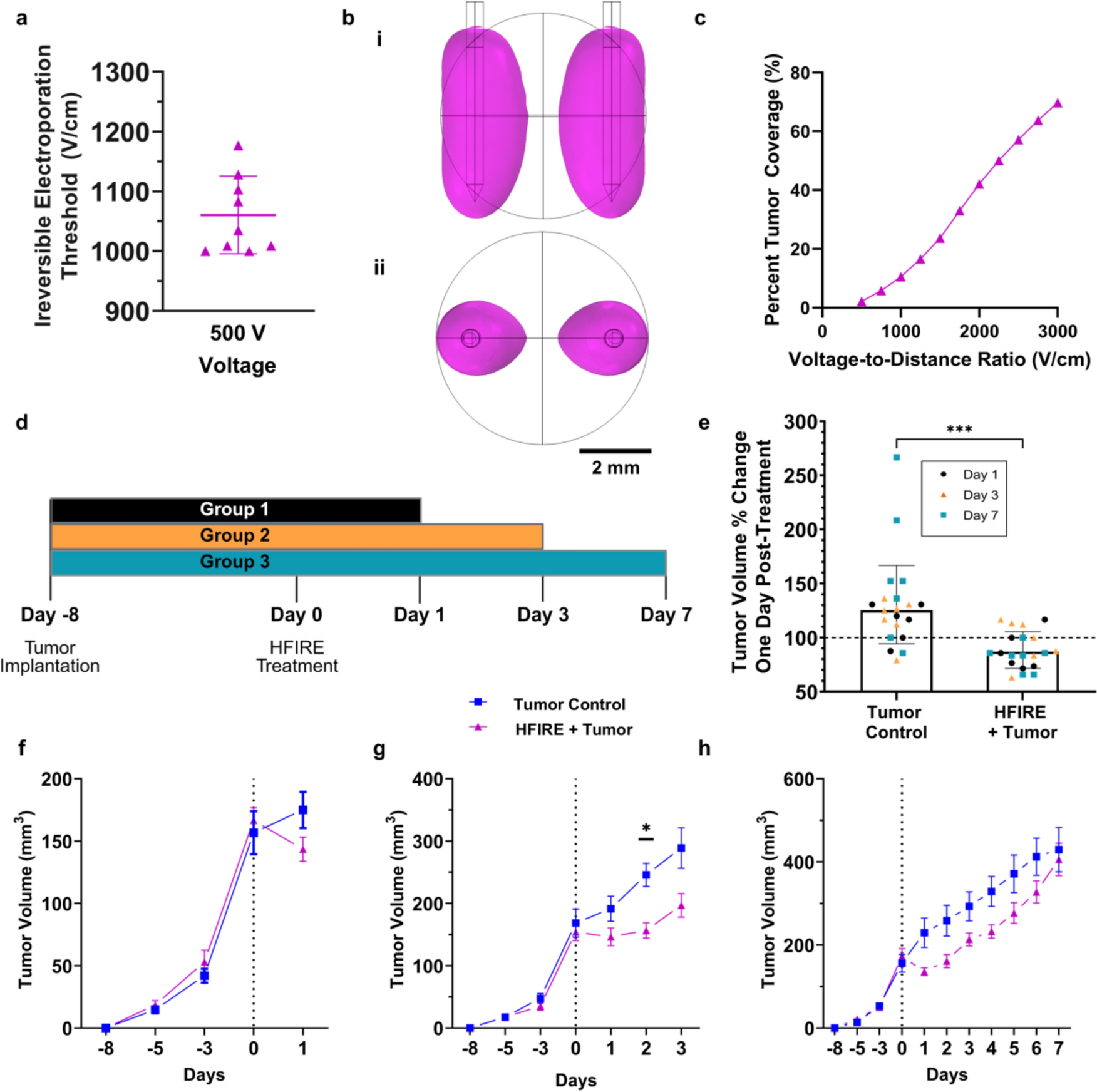
High-frequency irreversible electroporation (H-FIRE) is a minimally invasive local ablation therapy known to activate the adaptive immune system and reprogram the tumor microenvironment. Its predecessor, irreversible electroporation (IRE), transiently increases microvascular density and immune cell infiltration within the surviving non-ablated and non-necrotic tumor region, also known as the viable tumor region. However, the impact of pulse electric field therapies on lymphatic vessels, crucial for T-cell fate and maturation, remains unclear. This study investigates how sub-ablative H-FIRE (SA-HFIRE) affects lymphatic and blood microvascular remodeling in the 4T1 mammary mouse model. We conducted a temporal and spatial analysis to evaluate vascular changes in the viable tumor, peritumoral fat pad, and tumor-draining lymph node post-treatment. Histological examination showed a transient increase in blood vessel density on Day 1 post-treatment, followed by a spike in lymphatic vessel density in the viable tumor region on Day 3 post-treatment, increased lymphatic vessel density in the peripheral fat pad, and minimal remodeling of the tumor-draining lymph node within 3 days following treatment. Gene expression analysis indicated elevated levels of CCL21 and CXCL2 on Day 1 post-treatment, while VEGFA and VEGFC did not appear to contribute to vascular remodeling. Likewise, CCL21 protein content in tumor-draining axillary lymph nodes correlated with gene expression data from the viable tumor region. These findings suggest a dynamic shift in lymphatic and blood microvascular structures post-SA-HFIRE, potentially enhancing the adaptive immune response through CCL21-mediated lymphatic homing and subsequent lymph node microvascular remodeling. Future work will assess the immune and transport function of the microvasculature to inform experiments aimed at the application of adjuvant therapies during scenarios of tumor partial ablation.