2025-04-23 オックスフォード大学
<関連情報>
- https://www.ox.ac.uk/news/2025-04-23-new-study-finds-common-virus-may-improve-skin-cancer-treatment-outcomes
- https://www.nature.com/articles/s41591-025-03647-1
CMV血清ステータスは、抗PD-1チェックポイント阻害療法後の生存率改善および毒性発現遅延と関連する CMV serostatus is associated with improved survival and delayed toxicity onset following anti-PD-1 checkpoint blockade
Gusztav Milotay,Martin Little,Robert A. Watson,Dylan Muldoon,Sophie MacKay,Ayako Kurioka,Orion Tong,Chelsea A. Taylor,Isar Nassiri,Louisa M. Webb,Oluwafemi Akin-Adigun,Julia Bremke,Weiyu Ye,Bo Sun,Piyush Kumar Sharma,Ros Cooper,Sara Danielli,Flavia Matos Santo,Alba Verge de Los Aires,Guangyi Niu,Lea Cohen,Esther Ng,James J. Gilchrist,Amanda Y. Chong,… Benjamin P. Fairfax
Nature Medicine Published:23 April 2025
DOI:https://doi.org/10.1038/s41591-025-03647-1
Abstract
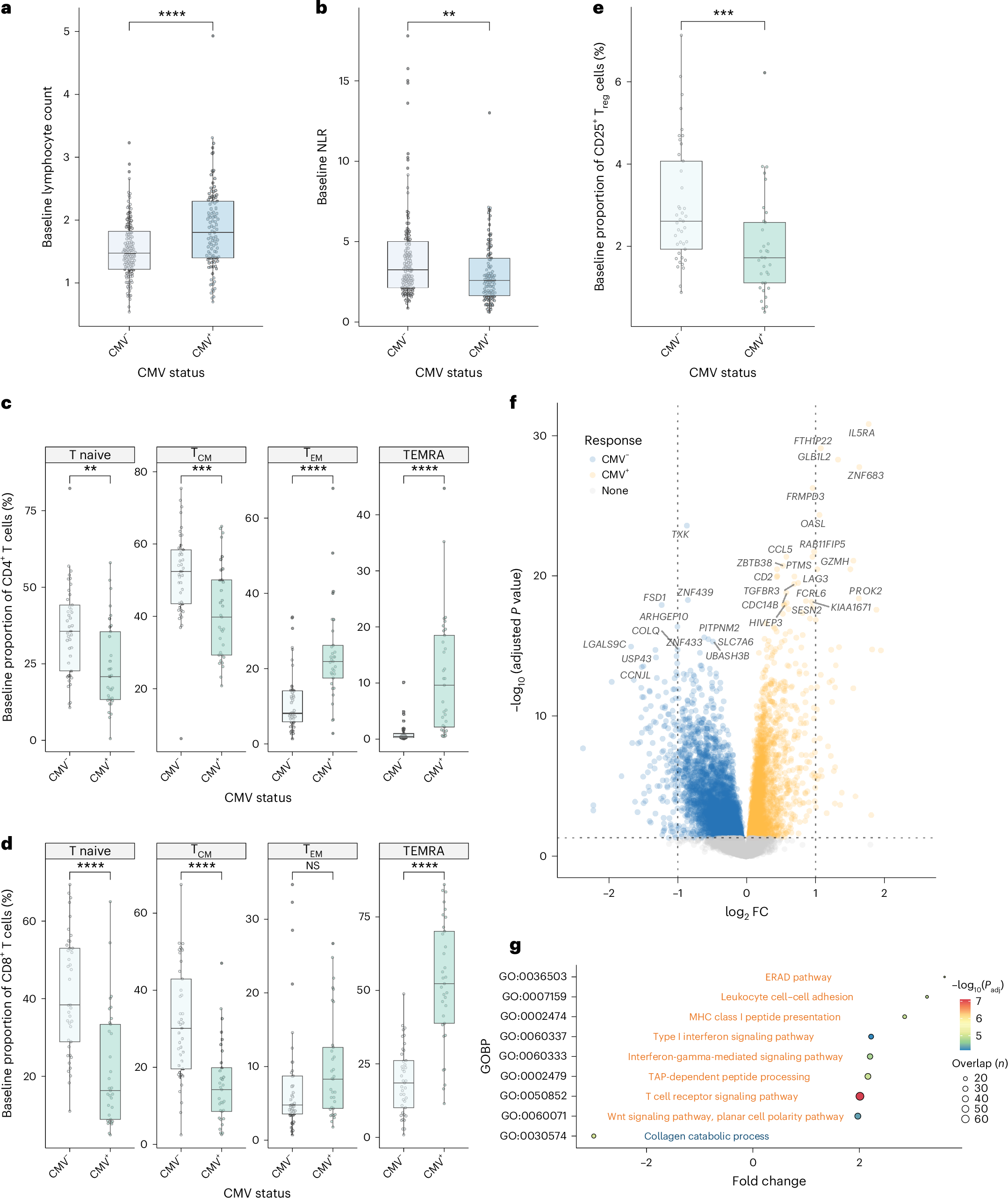
Cytomegalovirus (CMV) is a globally endemic latent herpes virus that profoundly impacts T cell immunity. We investigated the oncological consequences of CMV infection across 341 prospectively recruited patients receiving immune checkpoint blockade (ICB) for melanoma. CMV+ patients with metastatic melanoma (MM) have higher lymphocyte counts, reduced neutrophil to lymphocyte ratio and divergent CD8+ T cell gene expression. Combination anti-CTLA-4/anti-PD-1 ICB, but not single-agent anti-PD-1 ICB, induces cytotoxicity and CMV-associated gene expression in CD8+ T cells from CMV– patients. Correspondingly, overall survival was independent of CMV serostatus in combination anti-CTLA-4/anti-PD-1 ICB recipients (CMV+ hazard ratio for death: 1.02, P = 0.92), whereas CMV+ single-agent anti-PD-1 ICB recipients had improved overall survival (CMV+ hazard ratio for death: 0.37, P < 0.01), a finding also seen in CMV+ adjuvant single-agent anti-PD-1 ICB recipients (CMV+ hazard ratio for recurrence: 0.19, P = 0.03). We identify TBX21, encoding T-bet, as a transcriptional driver of CMV-associated CD8+ T cell gene expression, finding that TBX21 expression is predictive of overall survival (hazard ratio: 0.62, P = 0.026). CMV+ patients unexpectedly show reduced cumulative incidence of grade 3+ immune-related adverse events at 6 months (0.30 versus 0.52, P = 2.2 × 10-5), with lower incidence of colitis (P = 7.8 × 10-4) and pneumonitis (P = 0.028), an effect replicated in non-melanoma ICB recipients (n = 58, P = 0.044). Finally, we find reduced CMV seropositivity rates in patients with MM compared with UK Biobank controls (odds ratio: 0.52, P = 1.8 × 10-4), indicating CMV seropositivity may protect against MM. Specifically, patients with BRAF-mutated MM are less likely to be CMV+ (odds ratio = 2.2, P = 0.0054), while CMV– patients present 9 yr earlier with BRAF wild-type MM (P = 1.3 × 10-4). This work reveals an interaction between CMV infection, MM development according to BRAF status and response to ICB, while demonstrating CMV infection is protective against severe ICB immune-related adverse events, highlighting the potential importance of previous infection history and chronic immune activation in MM development and immunotherapy outcomes.


