2025-09-09 スイス連邦工科大学ローザンヌ校(EPFL)
<関連情報>
- https://actu.epfl.ch/news/gene-of-rare-disease-controls-post-injury-gut-rege/
- https://www.embopress.org/doi/full/10.1038/s44321-025-00295-3
損傷誘発性腸管幹細胞更新には毛細血管形成遺伝子2が必要である Injury-induced intestinal stem cell renewal requires capillary morphogenesis gene 2
Lucie Bracq, Audrey Chuat, Béatrice Kunz, Olivier Burri, Romain Guiet, Julien Duc, Nathalie Brandenberg, and F Gisou van der Goot
EMBO Molecular Medicine Published:22 August 2025
DOI:https://doi.org/10.1038/s44321-025-00295-3
Abstract
Patients with the rare genetic disorder Hyaline Fibromatosis Syndrome (HFS) often succumb before 18 months of age due to severe diarrhea. As HFS is caused by loss-of-function mutations in the gene encoding capillary morphogenesis gene 2 (CMG2), these symptoms highlight a critical yet unexplored role for CMG2 in the gut. Here, we demonstrate that CMG2 knockout mice exhibit normal colon morphology and no signs of inflammation until the chemical induction of colitis. In these conditions, the colons of knockout mice do not regenerate despite previously experiencing similarly severe colitis, due to an inability to replenish their intestinal stem cell pool. Specifically, CMG2 knockout impairs the transition from fetal-like to Lgr5+ adult stem cells, which is associated with a defect in ß-catenin nuclear translocation. Based on our findings, we propose that CMG2 functions as a context-specific modulator of Wnt signaling, essential for replenishing the pool of intestinal stem cells following injury. This study provides new insights into the molecular mechanisms underlying lethal diarrhea in HFS and offers a broader understanding of fetal-like regenerative responses.
Synopsis
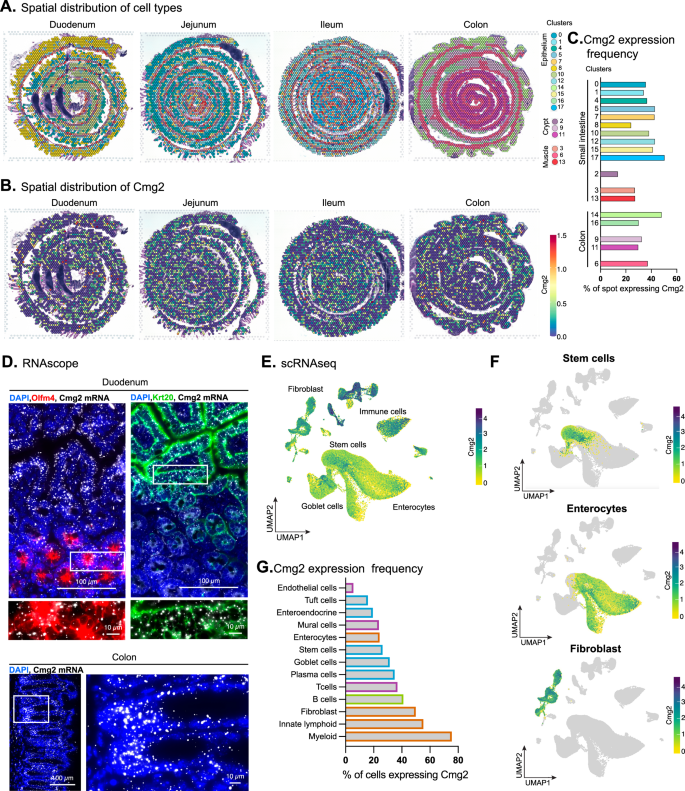
Hyaline Fibromatosis Syndrome (HFS) is caused by mutations in the CMG2 gene. Full loss of function mutations lead to death around 18 months due to recurrent diarrhea of unknown origin. We used a mouse model of HFS to investigate the molecular function of CMG2 in the gut.
- The gut of CMG2KO mice does not show any apparent alterations under homeostatic conditions.
- In a DSS-induced colitis model, CMG2KO mice exhibit gut regeneration failure after injury.
- This regeneration failure is linked to the conversion step from fetal-like stem cells to intestinal stem cells.
- Patients suffering from HFS could benefit from treatments established for other intestinal diseases, such as inflammatory bowel disease or Crohn’s disease.
The paper explained
Problem
Hyaline Fibromatosis Syndrome (HFS) is one of over 7000 known rare human diseases and is caused by mutations in the Capillary Morphogenesis Gene 2 (CMG2). Depending on the nature of the mutation, symptoms range from debilitating to fatal, with the most severe cases leading to death in infancy due to recurrent intractable diarrhea. The cause of this intestinal dysfunction has remained unknown, and a role for CMG2 in gut physiology has not been documented. In this study, we investigated the function of CMG2 in the intestine using a knockout mouse model of HFS.
Results
Unexpectedly, CMG2 knockout (CMG2KO) mice showed no signs of intestinal dysfunction under normal conditions: their gut morphology, weight, and overall health appeared normal. However, the intestine’s ability to regenerate after injury—an essential function of the gut—was severely impaired. Using a well-established model of chemically induced colitis (DSS treatment followed by withdrawal), we observed that while wild-type mice recovered fully, CMG2KO mice failed to regenerate their colonic epithelium. Further analysis revealed that the transition from fetal-like cells to Lgr5+ intestinal stem cells—a Wnt-dependent step critical for regeneration—was disrupted in the absence of CMG2.
Impact
This study uncovers a previously unrecognized role for CMG2 in intestinal regeneration and provides a molecular explanation for the severe diarrheal symptoms seen in HFS patients. These insights raise the possibility that patients with HFS could benefit from treatments currently used in other regenerative or inflammatory gut diseases, such as inflammatory bowel disease or Crohn’s disease.