2025-11-03 中山大学(SYSU)
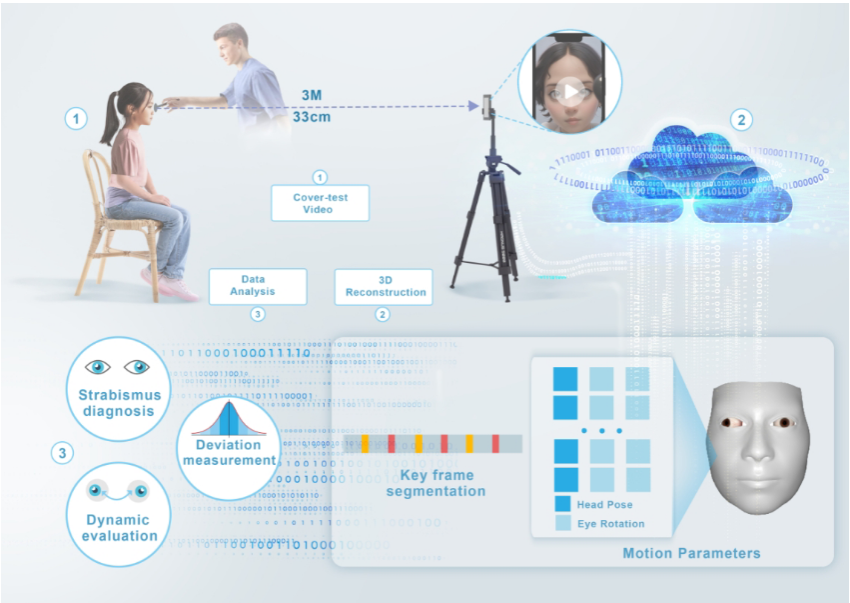
Workflow of the Digital Ruler of Strabismus System.
<関連情報>
スマートフォンベースのデジタル定規による眼科医レベルの斜視自動測定:前向き多施設コホート研究 A Smartphone-Based Digital Ruler to Automatically Measure Strabismus in Ophthalmologist-Level: A Prospective, Multicenter Cohort Study
Ruixin Wang, M.D., Ph.D., Junfeng Lyu, Ph.D., Yahan Yang, M.D., Ph.D., Shaowei Bi, M.Sc., M.D., Huanyun Yu, M.D., Ph.D., Hongwei Deng, M.D., Ph.D., Mengya Han, M.Sc., M.D., +5 , and Haotian Lin, M.D., Ph.D.
New England Journal of Medicine AI Published: October 23, 2025
DOI: 10.1056/AIoa2401205
Abstract
Background
Strabismus is a common condition that requires early screening to prevent amblyopia and stereopsis loss. Traditional methods are labor-intensive and costly, limiting their use. A smartphone-based approach for precise, automated strabismus measurement may offer a more accessible solution for early detection and management.
Methods
We developed the Digital Ruler of Strabismus (DRS), a system that employs three-dimensional reconstruction and deep learning algorithms to analyze 30-second videos of programmatic cover tests recorded by patients using smartphones. The diagnostic and quantitative performance of DRS was evaluated, and its consistency with manual prism measurements performed by ophthalmologists was compared.
Results
A total of 335 participants and 459 videos were collected from three eye centers, with ages ranging from 3 to 72 years. DRS demonstrated a mean absolute error of 4.51 prism diopters (PD) compared with the prism and alternate cover test, indicating good measurement performance. For horizontal deviation, it showed excellent agreement with the prism and alternate cover test, with an intraclass correlation coefficient of 0.98 (95% confidence interval [CI], 0.98 to 0.99). The Bland–Altman analysis further confirmed this agreement, with a mean difference of -1.1 PD and 95% limits of agreement ranging from -11.5 to 9.4 PD, which falls within the clinically acceptable range. With high sensitivity (0.974; 95% CI, 0.949 to 0.987) and specificity (0.938; 95% CI, 0.872 to 0.972), the DRS classification reliably differentiates phoria and tropia from normal ocular alignment. In addition, for intermittent strabismus, DRS can dynamically reconstruct the realignment time and speed during the examination, offering a novel method for observing and measuring the disease dynamics.
Conclusions
DRS enables strabismus assessment from videos recorded on consumer-grade smartphones. This approach may complement conventional clinic-based examinations and has the potential to expand access to strabismus screening and longitudinal monitoring, particularly in resource-limited settings. (Funded by the National Natural Science Foundation of China; ClinicalTrials.gov number, NCT05615519 and others.)