2026-01-15 岡山大学,国立がん研究センター,東北大学,島根大学
<関連情報>
- https://www.okayama-u.ac.jp/tp/release/release_id1486.html
- https://www.okayama-u.ac.jp/up_load_files/press_r7/press20260115-1.pdf
- https://onlinelibrary.wiley.com/doi/10.1111/acps.70065
統合失調症スペクトラム障害が大腸癌に対する侵襲的・全身的治療の受容に及ぼす影響:日本における全国多施設共同後ろ向きコホート研究 Impact of Schizophrenia Spectrum Disorders on the Receipt of Invasive and Systemic Therapy for Colorectal Cancer: A Nationwide Multicenter Retrospective Cohort Study in Japan
Masaki Fujiwara, Yuto Yamada, Taisuke Ishii, Tomone Watanabe, Maiko Fujimori, Naoki Nakaya, Toshihiko Kawamura, Koji Otsuki, Kunitoshi Shigeyasu, Taichi Shimazu, Shiro Hinotsu …
Acta Psychiatrica Scandinavica Published: 14 January 2026
DOI:https://doi.org/10.1111/acps.70065
ABSTRACT
Introduction
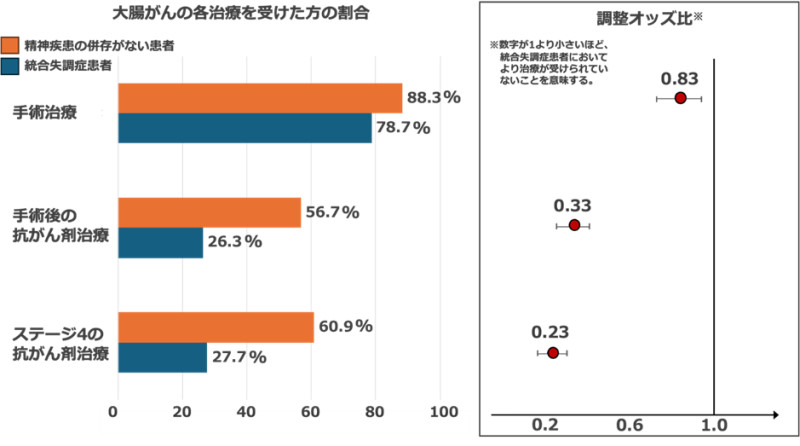
This study examined treatment disparities for colorectal cancer among patients diagnosed with schizophrenia spectrum disorders (SSD), focusing on invasive treatments and stage-appropriate systemic therapy within a universal healthcare system.
Method
In this nationwide retrospective cohort study (2018–2021), we identified 248,966 colorectal cancer patients, including 2337 diagnosed with SSD, using linked cancer registry and insurance claims data in Japan. The presence of SSD was classified according to ICD-10 codes F20–29. We used multivariable logistic regression to compare the odds of receiving stage-appropriate adjuvant chemotherapy and systemic therapy, as well as the odds of receiving surgical or endoscopic treatments, between the two groups. The analysis adjusted for age, sex, clinical stage, and scores on the Charlson Comorbidity Index and Barthel Index.
Results
The clinical stage distribution at diagnosis for colorectal cancer differed significantly between patients with SSD and those without psychiatric disorders (p < 0.001). After adjusting for clinical stage and other covariates, patients with SSD demonstrated significantly lower odds of receiving surgical or endoscopic treatment (adjusted odds ratio [aOR], 0.83; 95% CI, 0.73–0.94). The disparities were more pronounced for systemic therapy; patients with SSD had substantially lower odds of receiving adjuvant chemotherapy for stage III disease (aOR, 0.33; 95% CI, 0.26–0.41) and systemic therapy for stage IV disease (aOR, 0.23; 95% CI, 0.17–0.31).
Conclusion
Patients with SSD encounter substantial disparities in accessing standard colorectal cancer care, particularly systemic therapies. These findings highlight the urgent need for interventions to ensure equitable cancer treatment for this vulnerable population.
Summary
- Significant outcomes
- Patients diagnosed with schizophrenia spectrum disorders (SSD) were significantly less likely to receive surgical or endoscopic treatment for colorectal cancer compared with patients without psychiatric disorders.
- Disparities were particularly pronounced for systemic therapy; patients with SSD had markedly lower odds of receiving guideline-recommended adjuvant chemotherapy (stage III) and systemic therapy (stage IV).
- These findings highlight the urgent need for interventions to ensure equitable access to colorectal cancer treatment for patients with SSD, even in the context of a universal healthcare system.
- Limitations
- Survival outcomes were not available; therefore, the impact of treatment disparities on mortality could not be assessed.
- As the reasons for not receiving treatment were unknown, it was not possible to distinguish between medically justified decisions, patient preferences, and disparities in access to care.