2026-01-23 京都大学

<関連情報>
- https://www.kyoto-u.ac.jp/ja/research-news/2026-01-23-8
- https://www.kyoto-u.ac.jp/sites/default/files/2026-01/web_2601_Jo-c9a7ce357aeb54d955ca6c31b23055da.pdf
- https://www.isct-cytotherapy.org/article/S1465-3249(26)00021-6/fulltext
CAR-T細胞療法における点滴時の網状赤血球数の低下はICANSのリスク因子である Low Reticulocyte Count at Infusion is a Risk Factor for ICANS in CAR-T Cell Therapy
Yusuke Tashiro ∙ Tomoyasu Jo ∙ Toshio Kitawaki ∙ … ∙ Miki Nagao ∙ Akifumi Takaori-Kondo ∙ Yasuyuki Arai , …
Cytotherapy Published:January 17, 2026
DOI:https://doi.org/10.1016/j.jcyt.2026.102065
Highlights
- Low reticulocyte counts at infusion predict ICANS risk after CAR-T therapy.
- A history of CNS involvement and Axi-cel use were confirmed as ICANS risks.
- Even in grade 1 CRS, prolonged fever is a risk factor for ICANS.
ABSTRACT
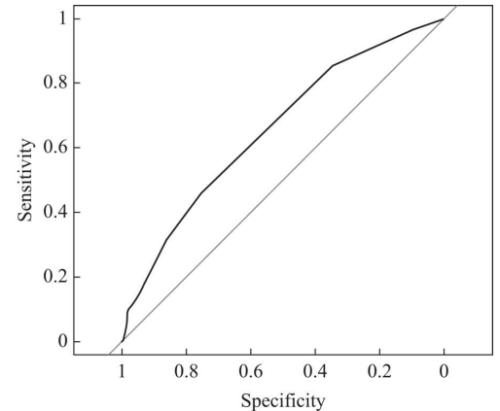
Chimeric antigen receptor (CAR)-T cell therapies targeting CD19 have shown efficacy against B-cell malignancies. However, they frequently cause immune effector cell-associated neurotoxicity syndrome (ICANS), which can be life-threatening and require intensive care. Even when it is not severe, ICANS can lead to prolonged hospitalization and limit treatment options, especially for elderly patients. Despite its clinical significance, a reliable, early predictive marker for ICANS has not been identified. To identify risk factors for ICANS, we retrospectively analyzed B-cell lymphoma patients who received tisagenlecleucel (tisa-cel), lisocabtagene maraleucel (liso-cel), or axicabtagene ciloleucel (axi-cel) at Kyoto University Hospital from 2019 to 2024. Among 106 patients, 76 received tisa-cel, 22 liso-cel, and 8 axi-cel. Median age at infusion was 63.5 years (interquartile range, 57–69). Eight patients (8%) had a history of central nervous system (CNS) involvement. ICANS occurred in 17 patients (16%), all with prior cytokine-release syndrome (CRS). Reticulocyte counts at infusion were significantly lower in patients who subsequently developed ICANS (1.57 vs. 2.80 × 104/μL, p<0.01). Multivariate analysis identified a low reticulocyte count at infusion (HR, 3.67; 95% CI, 1.23–11.02; p=0.02), history of CNS involvement (HR 8.37; 95% CI, 3.04–23.04; p<0.01), and axi-cel (HR, 4.56; 95% CI, 1.88–11.09; p<0.01) as independent risk factors. Patients divided by the median reticulocyte count at infusion (2.57 × 104/μL) demonstrated significantly higher 30-day cumulative incidence of ICANS in those with lower counts (25.5% vs. 7.8% at 30 days; p=0.018). Reticulocyte counts at infusion, a simple hematological parameter, may help predict ICANS development and guide optimal risk-based management of CAR-T cell therapy.