2023-09-27 バッファロー大学(UB)
◆この研究は、肥満手術後の成績を最適化するために精密医療が有用であることを強調しています。遺伝子情報と心理学的データを組み合わせて、患者ごとにカスタマイズされた治療アプローチを提供し、成功の要因や障害を克服する方法を特定するのに役立つと期待されています。
<関連情報>
- https://www.buffalo.edu/news/releases/2023/09/Genetics-predict-bariatric-surgery-how-patients-fare.html
- https://www.mdpi.com/2227-9059/11/10/2644
- https://www.mdpi.com/2075-4426/13/7/1164
1年後の肥満手術成績の予測因子としての遺伝的相関関係 Genetic Correlates as a Predictor of Bariatric Surgery Outcomes after 1 Year
Panayotis K. Thanos,Colin Hanna,Abrianna Mihalkovic,Aaron Hoffman,Alan Posner,John Butsch,Kenneth Blum,Lesley Georger,Lucy D. Mastrandrea and Teresa Quattrin
Biomedicines Published: 27 September 2023
DOI:https://doi.org/10.3390/biomedicines11102644
Abstract
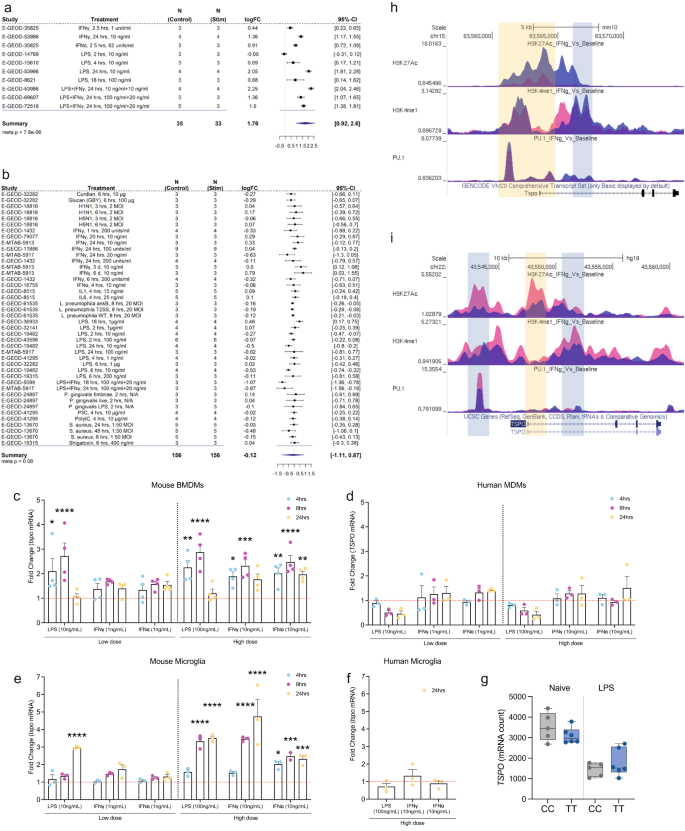
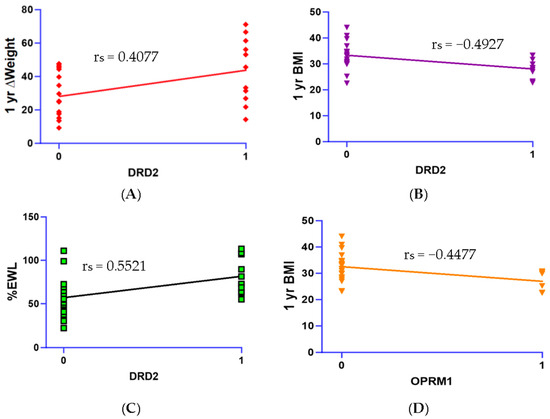
This study analyzed genetic risk assessments in patients undergoing bariatric surgery to serve as a predictive factor for weight loss parameters 1 year after the operation. Thirty (30) patients were assessed for Genetic Addiction Risk Severity (GARS), which analyzes neurogenetic polymorphisms involved in addiction and reward deficiency. Genetic and psychosocial data collected before the operation were correlated with weight loss data, including changes in weight, body mass index (BMI), and percent of expected weight loss (%EWL). Results examined correlations between individual gene risk alleles, 1-year body weight data, and psychosocial trait scores. Spearman’s correlations revealed that the OPRM1 (rs1799971) gene polymorphism had significant negative correlation with 1-year weight (rs = -0.4477, p < 0.01) and BMI (rs = -0.4477, p < 0.05). In addition, the DRD2 risk allele (rs1800497) was correlated negatively with BMI at 1 year (rs = -0.4927, p < 0.05), indicating that one risk allele copy was associated with lower BMI. However, this allele was positively correlated with both ∆Weight (rs = 0.4077, p < 0.05) and %EWL (rs = 0.5521, p < 0.05) at 1 year post-surgery. Moreover, the overall GARS score was correlated with %EWL (rs = 0.4236, p < 0.05), ∆Weight (rs = 0.3971, p < 0.05) and ∆BMI (rs = 0.3778, p < 0.05). Lastly, Food Cravings Questionnaire (FCQ) scores were negatively correlated with %EWL (rs = -0.4320, p < 0.05) and ∆Weight at 1 year post-surgery (rs = -0.4294, p < 0.05). This suggests that individuals with a higher genetic addiction risk are more responsive to weight loss treatment, especially in the case of the DRD2 polymorphism. These results should translate clinically to improve positivity and attitude related to weight management by those individuals born with the risk alleles (rs1800497; rs1799971).
心理社会的および遺伝的リスク評価を活用した、肥満手術の転帰を改善するための初の探索的個別化医療アプローチ: 臨床研究の奨励 The First Exploratory Personalized Medicine Approach to Improve Bariatric Surgery Outcomes Utilizing Psychosocial and Genetic Risk Assessments: Encouraging Clinical Research
Panayotis K. Thanos,Colin Hanna,Abrianna Mihalkovic,Aaron B. Hoffman,Alan R. Posner,John Busch,Caroline Smith,Rajendra D. Badgaiyan,Kenneth Blum,David Baron,Lucy D. Mastrandrea and Teresa Quattrin
Journal of Personalized Medicine Published: 20 July 2023
DOI:https://doi.org/10.3390/jpm13071164
Abstract
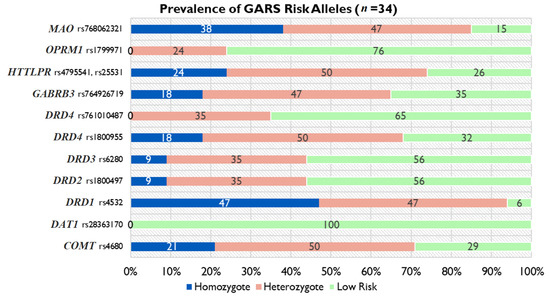
It is predicted that by 2030, globally, an estimated 2.16 billion adults will be overweight, and 1.12 billion will be obese. This study examined genetic data regarding Reward Deficiency Syndrome (RDS) to evaluate their usefulness in counselling patients undergoing bariatric surgery and gathered preliminary data on the potential use in predicting short term (6-month) weight loss outcomes. Methods: Patients undergoing bariatric surgery (n = 34) were examined for Genetic Addiction Risk Severity (GARS) [measures the presence of risk alleles associated with RDS]; as well as their psychosocial traits (questionnaires). BMI changes and sociodemographic data were abstracted from Electronic Health Records. Results: Subjects showed ∆BMI (M = 10.0 ± 1.05 kg/m2) and a mean % excess weight loss (56 ± 13.8%). In addition, 76% of subjects had GARS scores above seven. The homozygote risk alleles for MAO (rs768062321) and DRD1 (rs4532) showed a 38% and 47% prevalence among the subjects. Of the 11 risk alleles identified by GARS, the DRD4 risk allele (rs1800955), was significantly correlated with change in weight and BMI six months post-surgery. We identified correlations with individual risk alleles and psychosocial trait scores. The COMT risk allele (rs4680) showed a negative correlation with EEI scores (r = -0.4983, p < 0.05) and PSQI scores (r = -0.5482, p < 0.05). The GABRB3 risk allele (rs764926719) correlated positively with EEI (r = 0.6161, p < 0.01) and FCQ scores (r = 0.6373, p < 0.01). The OPRM1 risk allele showed a positive correlation with the DERS score (r = 0.5228, p < 0.05). We also identified correlations between DERS and BMI change (r = 0.61; p < 0.01). Conclusions: These data support the potential benefit of a personalized medicinal approach inclusive of genetic testing and psychosocial trait questionnaires when counselling patients with obesity considering bariatric surgery. Future research will explore epigenetic factors that contribute to outcomes of bariatric surgery.