2025-05-07 カロリンスカ研究所(KI)
<関連情報>
- https://news.ki.se/researchers-restore-antibiotic-effect-in-the-event-of-resistance
- https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01226-1
バクテリオファージ由来のエンドリジンがβ-ラクタムおよびマクロライド耐性肺炎球菌感染症の抗生物質感受性を回復させるBacteriophage-derived endolysins restore antibiotic susceptibility in β-lactam- and macrolide-resistant Streptococcus pneumoniae infections
Niels Vander Elst,Kristine Farmen,Lisa Knörr,Lotte Merlijn & Federico Iovino
Molecular Medicine Published:05 May 2025
DOI:https://doi.org/10.1186/s10020-025-01226-1
Abstract
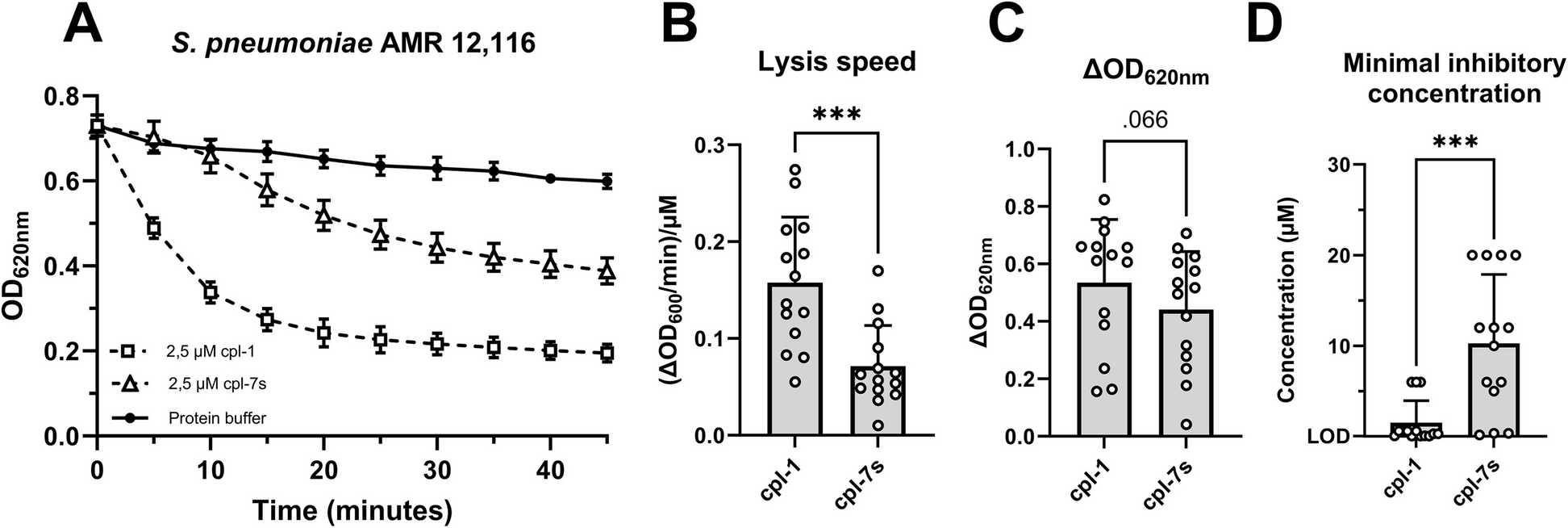
Streptococcus pneumoniae, the pneumococcus, is a cause of major illness globally. Invasive pneumococcal disease (IPD) is characterized by pneumococci invading blood (bacteremia), lungs (pneumonia), or brain and cerebrospinal fluid (meningitis). Meningitis remains an important global health concern because half of the survivors experience long-term neurological damage. The antibiotics commonly used to treat pneumococcal infections are β-lactams and macrolides, however, S. pneumoniae is nowadays often resistant to one or several antibiotics, therefore novel antimicrobials are needed. Here, we found that the bacteriophage-derived cpl-1 endolysin showed consistent antibacterial activity against β-lactam- and macrolide-resistant pneumococcal clinical strains grown in human blood and human cerebrospinal fluid. Exploiting synergistic and additive mechanisms, supplementation of cpl-1 to either penicillin or erythromycin, as representatives for β-lactam and macrolide antibiotics, rescued human neuronal cells from the cytotoxicity of antibiotic-resistant pneumococcal infections. Finally, systemic administration of cpl-1 supplemented to penicillin in mice infected with penicillin-resistant pneumococci successfully reduced bacteremia, and, thanks to the efficient penetration across the blood–brain barrier, abolished bacterial load in the brain, resulting in increased (89%) survival accompanied by an asymptomatic course of infection. These findings strongly suggest that cpl-1 can enhance antibiotic susceptibility in β-lactam- and macrolide-resistant S. pneumoniae, serving as a valuable adjunct therapy to standard-of-care antibiotics for multidrug-resistant IPD.


