2025-06-09 カリフォルニア大学サンフランシスコ校(UCSF)
<関連情報>
- https://www.ucsf.edu/news/2025/06/430141/how-high-your-dementia-risk-it-might-depend-where-you-live
- https://jamanetwork.com/journals/jamaneurology/article-abstract/2834952
米国退役軍人の認知症罹患率における地域差 Regional Differences in Dementia Incidence Among US Veterans
Christina S. Dintica, PhD; Amber L. Bahorik, PhD; Feng Xia, MPH; et al
JAMA Neurology Published:June 9, 2025
DOI:10.1001/jamaneurol.2025.1536
Key Points
Question Are there regional variations in dementia incidence across the US in a nationally representative sample?
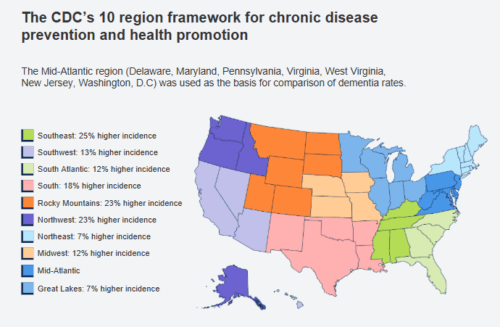
Findings In this cohort of 1 268 599 older US veterans, dementia incidence rates per 1000 person-years were lowest in the Mid-Atlantic (11.2) and highest in the Southeast (14.0); compared with the Mid-Atlantic, the regions with greatest demographically adjusted incidence included the Southeast (25% higher risk), Northwest (23% higher risk), and Rocky Mountains (23% higher risk), and rates for other regions were 7% to 18% higher. These differences persisted after adjustment for key covariates and competing risk of death.
Meaning These results underscore the influence of regionally patterned risk factors or diagnostic practices, highlighting the importance of tailored health care strategies, public health initiatives, and policy reforms.
Abstract
Importance Prior studies of dementia incidence in the US often focused on narrow regions, leaving regional variation unclear and potential explanatory factors unknown.
Objective To investigate geographic differences in dementia incidence across the US among older adults enrolled in the Veterans Health Administration (VHA) system.
Design, Setting, and Population Cohort study spanning October 1999 to September 2021 with a mean follow-up time of 12.6 years. Data were analyzed from October 2023 to September 2024 among a random sample of 1 268 599 dementia-free veterans aged 65 years or older with available zip code information in locations across the US. We excluded 22 512 with missing zip codes, 265 850 with no follow-up, and 37 370 with prevalent dementia.
Exposure Geographical region categories across the US were defined using the Centers for Disease Control and Prevention (CDC) National Center for Chronic Disease Prevention and Health Promotion definition, which divides the US into 10 regions, each composed of 4 to 7 states.
Main Outcomes and Measures Dementia diagnoses were based on International Classification of Diseases codes and calculated for zip codes within the CDC regions. Poisson regression models were used to calculate dementia incidence per 1000 person-years and assess regional differences in incidence rate ratios with several covariate models.
Results Among the 1 268 599 participants (mean age, 73.9 [SD, 6.1] years; n = 25 335 [2%] female), dementia incidence rates per 1000 person-years were lowest in the Mid-Atlantic (11.2; 95% CI, 11.1-11.4) and highest in the Southeast (14.0; 95% CI, 13.8-14.2). Compared with the Mid-Atlantic, the regions with the greatest demographically adjusted incidence included the Southeast (rate ratio [RR], 1.25; 95% CI, 1.22-1.28), Northwest (RR, 1.23; 95% CI, 1.20-1.27), Rocky Mountains (RR, 1.23; 95% CI, 1.20-1.26), South (RR, 1.18; 95% CI, 1.15-1.20), Midwest (RR, 1.12; 95% CI, 1.09-1.14), and South Atlantic (RR, 1.12; 95% CI, 1.10-1.14); the remaining regions had similar (<10% difference) incidence. Additional adjustments for rurality and cardiovascular comorbidities and accounting for the competing risk of death produced similar results.
Conclusions and Relevance Among older adults in the VHA, dementia incidence varied significantly across US regions, independent of key covariates. These findings highlight the need for targeted health care planning, public health interventions, and policy development.


