2025-07-18 東京大学
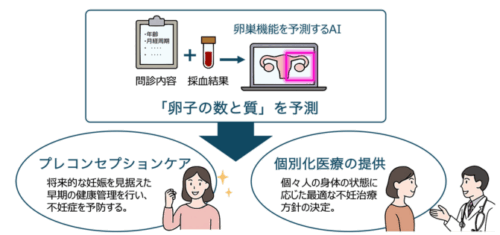
卵巣機能を予測する AI モデルの概略
<関連情報>
- https://www.h.u-tokyo.ac.jp/press/20250718.html
- https://www.h.u-tokyo.ac.jp/press/__icsFiles/afieldfile/2025/07/17/release_20250718.pdf
- https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01732-0
機械学習を用いた卵巣の量的・質的予備能の評価と予測モデル Assessment and prediction models for the quantitative and qualitative reserve of the ovary using machine learning
Hiroshi Koike,Miyuki Harada,Kaname Yoshida,Katsuhiko Noda,Chihiro Tsuchida,Toshihiro Fujiwara,Akari Kusamoto,Zixin Xu,Tsurugi Tanaka,Nanoka Sakaguchi,Chisato Kunitomi,Nozomi Takahashi,Yoko Urata,Kenbun Sone,Osamu Wada-Hiraike,Yasushi Hirota & Yutaka Osuga
Journal of Ovarian Research Published: 18 July 2025
DOI:https://doi.org/10.1186/s13048-025-01732-0
Abstract
Background
The age-related decline of fertility is caused by a reduction of the ovarian reserve, which is represented by the number and quality of oocytes in the ovaries. Anti-Müllerian hormone (AMH) is considered one of the most useful markers of the quantity of the ovarian reserve; however, a more accurate prediction method is required. Furthermore, there is no clinically useful tool to assess the quality of the ovarian reserve and therefore a prediction tool is required. Our aim is to produce a model for prediction of the ovarian reserve that contributes to preconception care and precision medicine.
Methods
This study was a retrospective analysis of 442 patients undergoing assisted reproductive technology (ART) treatment in Japan from June 2021 to January 2023. Medical records and residual serum of patients undergoing oocyte retrieval were collected. Binary classification models predicting the ovarian reserve were created using machine learning methods developed with many collected feature values. The best-performing model among 15 examined models was selected based on its area under the receiver operating characteristic curve (AUC) and accuracy. To maximize performance, feature values used for model creation were narrowed down and extracted.
Results
The best-performing model to assess the quantity of the ovarian reserve was the random forest model with an AUC of 0.9101. Five features were selected to create the model and consisted of data from only medical records. The best-performing model to assess the quality of the ovarian reserve was the random forest model, which had an AUC of 0.7983 and was created with 14 features, data from medical records and residual serum analysis.
Conclusion
Our models are more accurate than currently popular methods for predicting the ovarian reserve. Furthermore, they can assess the ovarian reserve using only information obtained from a medical interview and single blood sampling. Enabling easy measurement of the ovarian reserve with this model would allow a greater number of women to engage in preconception care and facilitate the delivery of personalized medical treatment for patients undergoing infertility therapy.
Clinical trial number
Not applicable.