2026-01-22 国立循環器病研究センター
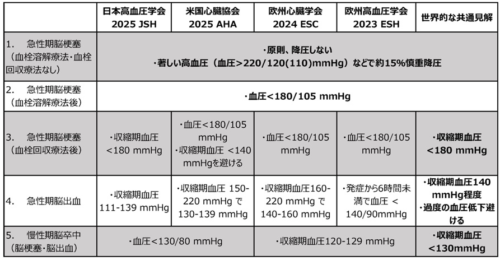
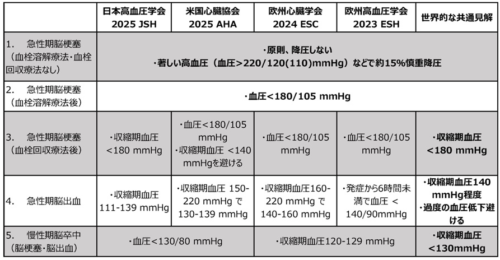
(表1)日米欧4ガイドラインの脳卒中血圧管理推奨の比較
<関連情報>
脳卒中における血圧管理:2025年AHA/ACC/AANP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM、2024年ESC、2023年ESH、および2025年JSHガイドラインの比較レビュー Blood pressure management in stroke: comparative review of the 2025 AHA/ACC/AANP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM, 2024 ESC, 2023 ESH, and 2025 JSH guidelines
Masatoshi Koga
Hypertension Research Published:09 January 2026
DOI:https://doi.org/10.1038/s41440-025-02517-0
The Original Article was published on 01 January 2026
Abstract
Hypertension is the primary modifiable risk factor for both ischemic stroke and intracerebral hemorrhage (ICH), yet recommendations for blood pressure (BP) management vary across contemporary guidelines. This narrative review compares BP targets and therapeutic strategies in the 2025 American Heart Association (AHA), 2024 European Society of Cardiology (ESC), 2023 European Society of Hypertension (ESH), and 2025 Japanese Society of Hypertension (JSH) guidelines, with emphasis on acute and chronic phases of ischemic stroke and ICH. In acute ischemic stroke without reperfusion therapy, all four guidelines discourage routine BP lowering unless systolic BP (SBP) is ≥220 mmHg or diastolic BP ≥ 120 (110) mmHg, and then recommend only modest reductions of about 15% within 24 hours. For patients receiving IV thrombolysis or mechanical thrombectomy, the guidelines converge on pre-treatment BP<185/110 mmHg and maintenance <180/105 mmHg during the first 24 hours, with JSH specifying micro-infusion calcium channel blockers as preferred agents. In chronic ischemic stroke, AHA, ESH, and JSH generally endorse BP<130/80 mmHg, whereas ESC prioritizes an SBP range of 120-9 mmHg. For acute ICH, all guidelines support rapid but carefully titrated SBP reduction toward approximately 140 mmHg, while emphasizing avoidance of overshoot, large variability, and excessive early declines, particularly when baseline SBP exceeds 220 mmHg in the AHA and ESC guidelines. Long-term after ICH, targets of <130/80 mmHg are widely recommended. Thiazide diuretics, ACE inhibitors, and angiotensin receptor blockers remain foundational for secondary prevention, with calcium channel blockers central to acute parenteral therapy and β-blockers reserved for specific indications. Despite regional nuances, the guidelines converge on conservative acute management in ischemic stroke, proactive early lowering in ICH, and intensive long-term BP control as the global benchmark for secondary cerebrovascular prevention.