2023-09-21 ペンシルベニア州立大学(PennState)
◆研究結果は、「ネイチャー・メディシン」誌に掲載されました。現在、アーテミシニン耐性が広まる可能性があるため、最適な治療法を待つのではなく、すぐに有効な治療政策を導入する必要があるとされています。研究では、ALと呼ばれるアーテミシニン系治療薬を3日から5日に延長し、複数の薬剤を同時に使用する2つの戦略が治療失敗率を10%以下に維持できる可能性があることが示されました。また、TACTs(三重アーテミシニン系治療薬)の導入が耐性の拡散を遅らせる可能性が高いことも明らかになりました。
<関連情報>
- https://www.psu.edu/news/research/story/new-strategies-may-reduce-treatment-failure-malaria-81/
- https://www.nature.com/articles/s41591-023-02551-w
- https://www.nature.com/articles/s41467-023-39914-3
ルワンダにおけるアルテミシニン耐性pfkelch R561H変異の拡散を遅らせるための政策介入をモデル化 Modeling policy interventions for slowing the spread of artemisinin-resistant pfkelch R561H mutations in Rwanda
Robert J. Zupko,Tran Dang Nguyen,J. Claude S. Ngabonziza,Michee Kabera,Haojun Li,Thu Nguyen-Anh Tran,Kien Trung Tran,Aline Uwimana & Maciej F. Boni
Nature Medicine Published:21 September 2023
DOI:https://doi.org/10.1038/s41591-023-02551-w
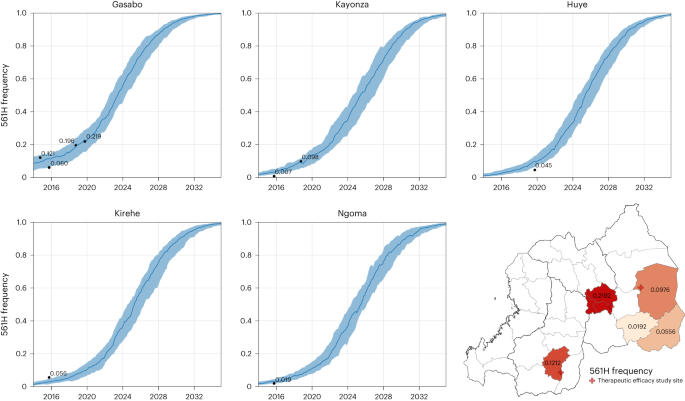
Abstract
Artemisinin combination therapies (ACTs) are highly effective at treating uncomplicated Plasmodium falciparum malaria, but the emergence of the new pfkelch13 R561H mutation in Rwanda, associated with delayed parasite clearance, suggests that interventions are needed to slow its spread. Using a Rwanda-specific spatial calibration of an individual-based malaria model, we evaluate 26 strategies aimed at minimizing treatment failures and delaying the spread of R561H after 3, 5 and 10 years. Lengthening ACT courses and deploying multiple first-line therapies (MFTs) reduced treatment failures after 5 years when compared to the current approach of a 3-d course of artemether–lumefantrine. The best among these options (an MFT policy) resulted in median treatment failure counts that were 49% lower and a median R561H allele frequency that was 0.15 lower than under baseline. New approaches to resistance management, such as triple ACTs or sequential courses of two different ACTs, were projected to have a larger impact than longer ACT courses or MFT; these were associated with median treatment failure counts in 5 years that were 81–92% lower than the current approach. A policy response to currently circulating artemisinin-resistant genotypes in Africa is urgently needed to prevent a population-wide rise in treatment failures.
アルテミシニンベースの3剤併用療法で抗マラリア薬耐性を防ぐ Preventing antimalarial drug resistance with triple artemisinin-based combination therapies
Tran Dang Nguyen,Bo Gao,Chanaki Amaratunga,Mehul Dhorda,Thu Nguyen-Anh Tran,Nicholas J. White,Arjen M. Dondorp,Maciej F. Boni & Ricardo Aguas
Nature Communications Published:29 July 2023
DOI:https://doi.org/10.1038/s41467-023-39914-3
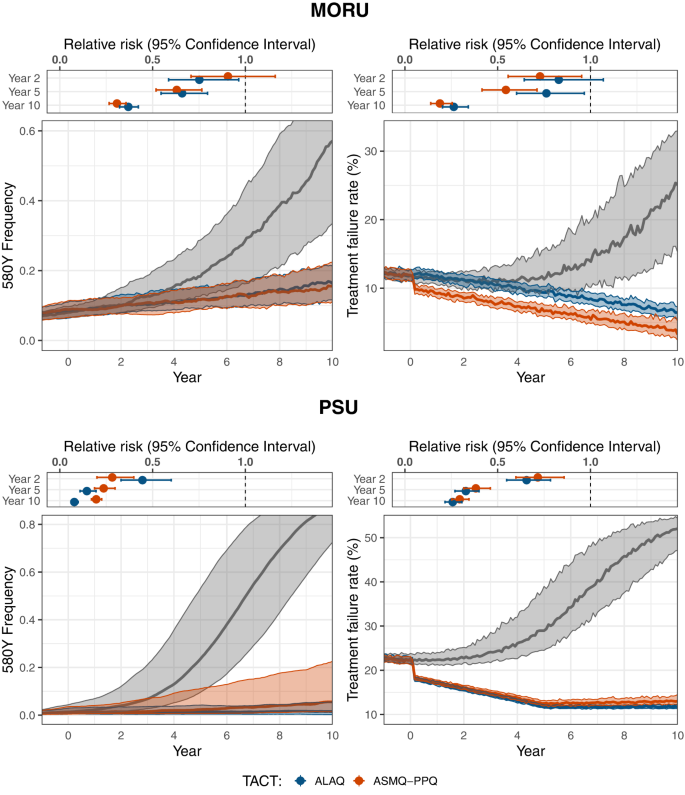
Abstract
Increasing levels of artemisinin and partner drug resistance threaten malaria control and elimination globally. Triple artemisinin-based combination therapies (TACTs) which combine artemisinin derivatives with two partner drugs are efficacious and well tolerated in clinical trials, including in areas of multidrug-resistant malaria. Whether early TACT adoption could delay the emergence and spread of antimalarial drug resistance is a question of vital importance. Using two independent individual-based models of Plasmodium falciparum epidemiology and evolution, we evaluated whether introduction of either artesunate-mefloquine-piperaquine or artemether-lumefantrine-amodiaquine resulted in lower long-term artemisinin-resistance levels and treatment failure rates compared with continued ACT use. We show that introduction of TACTs could significantly delay the emergence and spread of artemisinin resistance and treatment failure, extending the useful therapeutic life of current antimalarial drugs, and improving the chances of malaria elimination. We conclude that immediate introduction of TACTs should be considered by policy makers in areas of emerging artemisinin resistance.