2024-03-26 ジョージア工科大学
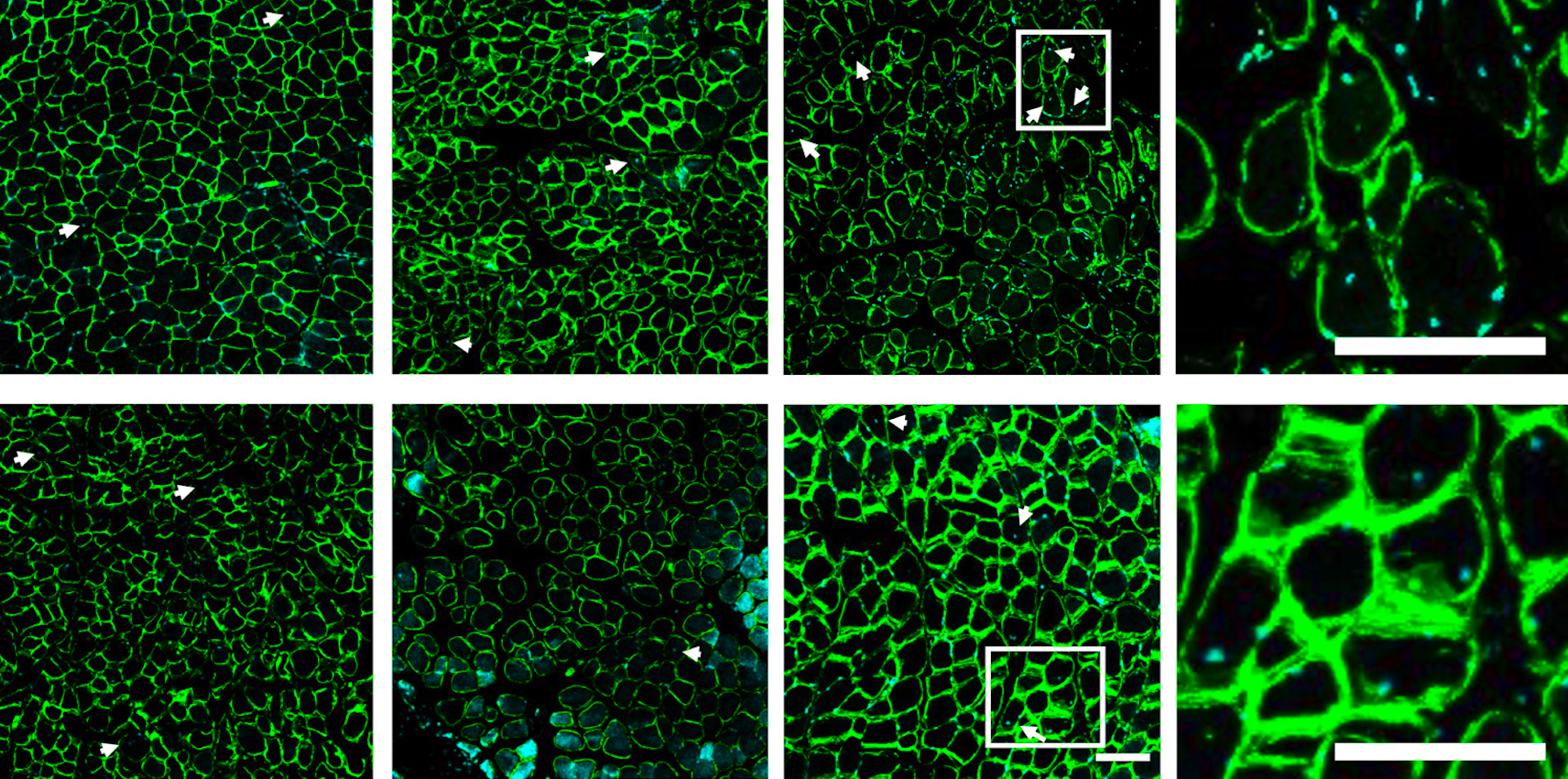
A combination of mobilizing agent, designed to “push” pro-healing cells into the blood, and SDF-1a, designed to “pull” the cells into the injury site, leads to an increase in muscle regeneration following a rotator cuff tear. Muscle regeneration was characterized based on the number of centrally located nuclei (marked with the white arrows).
<関連情報>
- https://research.gatech.edu/two-way-cell-based-treatment-repairs-muscle-after-rotator-cuff-injury
- https://www.liebertpub.com/doi/10.1089/ten.tea.2023.0128
骨髄動員および局所間質細胞由来因子-1α導入が棘上筋線維の成長を促進する Bone Marrow Mobilization and Local Stromal Cell-Derived Factor-1α Delivery Enhances Nascent Supraspinatus Muscle Fiber Growth
Leah E. Anderson, Liane E. Tellier, Keshav R. Shah, Joseph J. Pearson, Alexandra L. Brimeyer, Edward A. Botchwey, and Johnna S. Temenoff
Tissue Engineering Published:17 Jan 2024
DOI:https://doi.org/10.1089/ten.tea.2023.0128
Abstract
Rotator cuff tear is a significant problem that leads to poor clinical outcomes due to muscle degeneration after injury. The objective of this study was to synergistically increase the number of proregenerative cells recruited to injure rotator cuff muscle through a novel dual treatment system, consisting of a bone marrow mobilizing agent (VPC01091), hypothesized to “push” prohealing cells into the blood, and localized delivery of stromal cell-derived factor-1α (SDF-1α), to “pull” the cells to the injury site. Immediately after rotator cuff tendon injury in rat, the mobilizing agent was delivered systemically, and SDF-1α-loaded heparin-based microparticles were injected into the supraspinatus muscle. Regenerative and degenerative changes to supraspinatus muscle and the presence of inflammatory/immune cells, mesenchymal stem cells (MSCs), and satellite cells were assessed via flow cytometry and histology for up to 21 days. After dual treatment, significantly more MSCs (31.9 ± 8.0% single cells) and T lymphocytes (6.7 ± 4.3 per 20 × field of view) were observed in supraspinatus muscle 7 days after injury and treatment compared to injury alone (14.4 ± 6.5% single cells, 1.2 ± 0.7 per 20 × field of view), in addition to an elevated M2:M1 macrophage ratio (3.0 ± 0.5), an indicator of a proregenerative environment. These proregenerative cellular changes were accompanied by increased nascent fiber formation (indicated by embryonic myosin heavy chain staining) at day 7 compared to SDF-1α treatment alone, suggesting that this method may be a promising strategy to influence the early cellular response in muscle and promote a proregenerative microenvironment to increase muscle healing after severe rotator cuff tear.