2025-03-21 バーミンガム大学
<関連情報>
- https://www.birmingham.ac.uk/news/2025/nearly-half-of-depression-diagnoses-could-be-considered-treatment-resistant
- https://www.cambridge.org/core/journals/the-british-journal-of-psychiatry/article/examining-the-needs-outcomes-and-current-treatment-pathways-of-2461-people-with-treatmentresistant-depression-mixedmethods-study/429CA634F3B16949632EDCD9F2067430
治療抵抗性うつ病患者2461人のニーズ、転帰、現在の治療経路を検証する:混合方法研究 Examining the needs, outcomes and current treatment pathways of 2461 people with treatment-resistant depression: mixed-methods study
Kiranpreet Gill,Danielle Hett,Max Carlish,Rebekah Amos,Ali Khatibi,Isabel Morales-Muñoz andSteven Marwaha
The British Journal of Psychiatry Published:12 March 2025
DOI:https://doi.org/10.1192/bjp.2024.275
Abstract
Background
A substantial subset of patients with major depressive disorder (MDD) experience treatment-resistant depression (TRD), typically defined as failure to respond to at least two sequential antidepressant trials at adequate dose and length.
Aims
To examine clinical and service-level associations of TRD, and the experiences of people with TRD and clinicians involved in their care within a large, diverse National Health Service trust in the UK.
Method
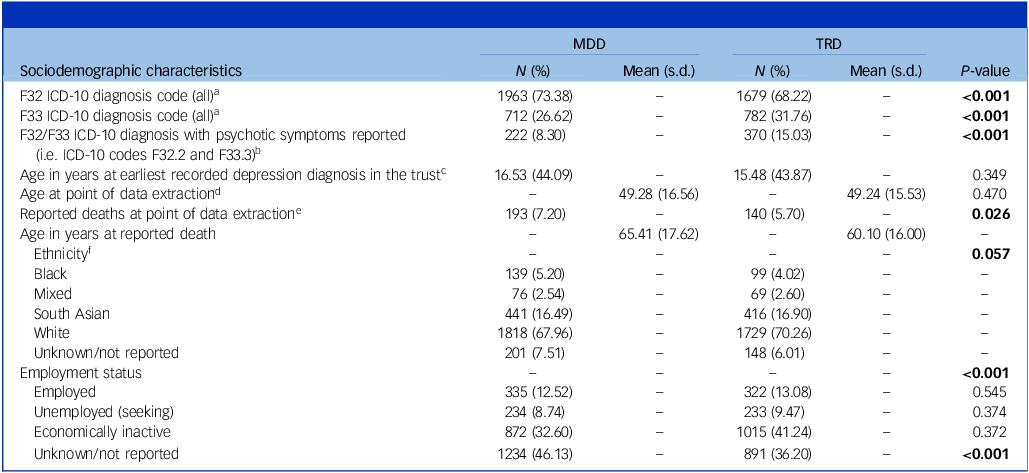
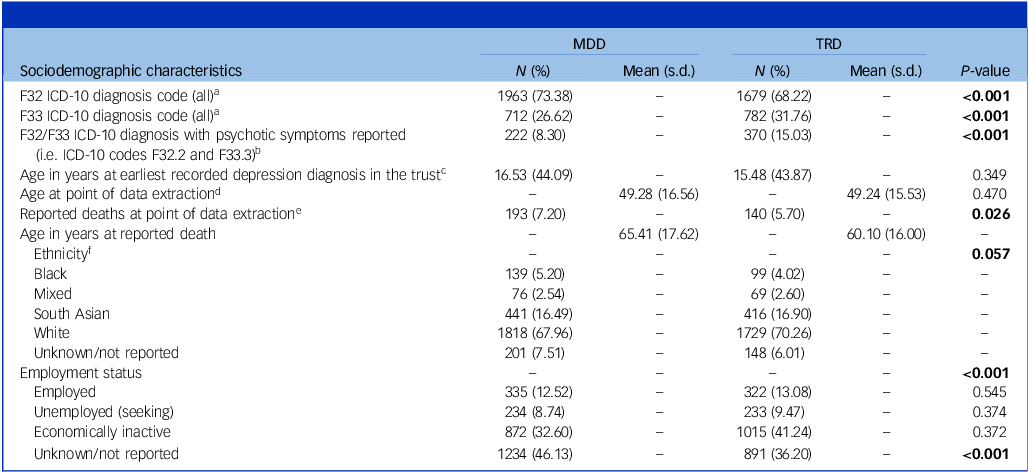
This mixed-methods study integrated quantitative analysis of electronic health records with thematic analysis of semi-structured interviews. Chi-squared tests and one-way analysis of variance were used to assess associations between lines of antidepressant treatments and sociodemographic and clinical variables, and binary logistic regression was used to identify associations of TRD status.
Results
Nearly half (48%) of MDD patients met TRD criteria, with 36.9% having trialled ≥4 antidepressant treatments. People with TRD had higher rates of recurrent depression (odds ratio = 1.24, 95% CI: 1.05–1.45, P = 0.008), comorbid anxiety disorders (odds ratio = 1.21, 95% CI: 1.03–1.41, P = 0.019), personality disorders (odds ratio=1.35, 95% CI: 1.10–1.65, P = 0.003), self-harm (odds ratio = 1.76, 95% CI: 1.06–2.93, P = 0.029) and cardiovascular diseases (odds ratio = 1.46, 95% CI: 1.02–2.07, P = 0.0374). Greater treatment resistance was linked to increased economic inactivity and functional loss. Qualitative findings revealed severe emotional distress and frustration with existing treatments, as well as organisational and illness-related barriers to effective care.
Conclusions
TRD is characterised by increasing mental and physical morbidity and functional decline, with individuals experiencing barriers to effective care. Improved pathways, service structures and more effective biological and psychological interventions are needed.