2025-03-27 国立成育医療研究センター
<関連情報>
- https://www.ncchd.go.jp/press/2025/0327.html
- https://link.springer.com/article/10.1007/s10384-023-01023-5
- https://link.springer.com/article/10.1007/s10384-025-01171-w
- https://bmjophth.bmj.com/content/9/1/e001713
5-35歳の日本人における後天性内斜視の臨床像とデジタル機器の使用:多施設登録データ解析研究 Clinical presentations of acquired comitant esotropia in 5–35 years old Japanese and digital device usage: a multicenter registry data analysis study
Hirohito Iimori,Sachiko Nishina,Osamu Hieda,Toshiaki Goseki,Noriko Nishikawa,Sadao Suzuki,Akiko Hikoya,Miwa Komori,Hiroko Suzuki,Tomoyo Yoshida,Shion Hayashi,Takafumi Mori,Akiko Kimura,Takeshi Morimoto,Yukiko Shimizu,Takashi Negishi,Tamami Shimizu,Yoshimi Yokoyama,Yoshiko Sugiyama,Noriyuki Azuma & Miho Sato
Japanese Journal of Ophthalmology Published:11 September 2023
DOI:https://doi.org/10.1007/s10384-023-01023-5
Abstract
Purpose
To describe clinical presentations of acquired comitant esotropia and digital device use in children, adolescents, and young adults without neurological problems.
Study design
Multicenter prospective observational study.
Methods
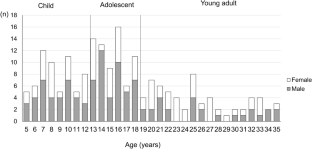
Patients with acquired comitant esotropia, without intracranial diseases aged 5–35 years at the time of visit, who were seen at pre-registered facilities within 1 year of onset were enrolled. The duration from the onset of symptoms and the time of digital device usage approximately 1 month before onset and their lifestyles were surveyed. Visual acuity, cycloplegic refraction, and strabismus angles were measured. Data were analyzed in three age groups (Child: 5–12 years, Adolescent: 13–18 years, and Young adult: 19–35 years).
Results
Between November 2019 and December 2021, 218 patients were enrolled from 55 facilities, and 194 patients (including 62 children, 69 adolescents, and 63 young adults) were analyzed. The child group spent the least amount of time using digital devices (children: 159; adolescents: 210; young adults: 267 min/work day, p < 0.05; (mean time in the same order below) 229, 338, 314 min/holiday, p < 0.05) and had the largest strabismus angle (mean strabismus angle at near: 30, 22, 18 PD, p < 0.01; at far: 28, 26, 21 PD, p<0.05).
Conclusion
The clinical features of acquired comitant esotropia and hand-held digital device usage differed between children aged ≤ 12 years and older patients. This report gives the current clinical characteristics of young patients with acquired esotropia and digital device usage.
デジタル機器の長期使用が後天性内斜視に及ぼす影響: ACE-DD研究2 Impact of prolonged digital device use on acquired comitant esotropia: ACE-DD study 2
Hirohito Iimori,Noriko Nishikawa,Sachiko Nishina,Tomoyo Yoshida,Takafumi Mori,Osamu Hieda,Akiko Hikoya,Miwa Komori,Shion Hayashi,Takashi Negishi,Toshiaki Goseki,Yoshiko Sugiyama,Akiko Kimura,Takeshi Morimoto,Yukiko Shimizu,Tamami Shimizu,Yoshimi Yokoyama,Hiroko Suzuki,Sadao Suzuki,Noriyuki Azuma & Miho Sato
Japanese Journal of Ophthalmology Published:17 March 2025
DOI:https://doi.org/10.1007/s10384-025-01171-w
Abstract
Purpose
To investigate changes in strabismus angles in children and young adult patients with recent onset of constant acquired comitant esotropia (ACE) following instructions on hand-held digital devices (DD).
Study design
Prospective multicenter non-randomized interventional study.
Methods
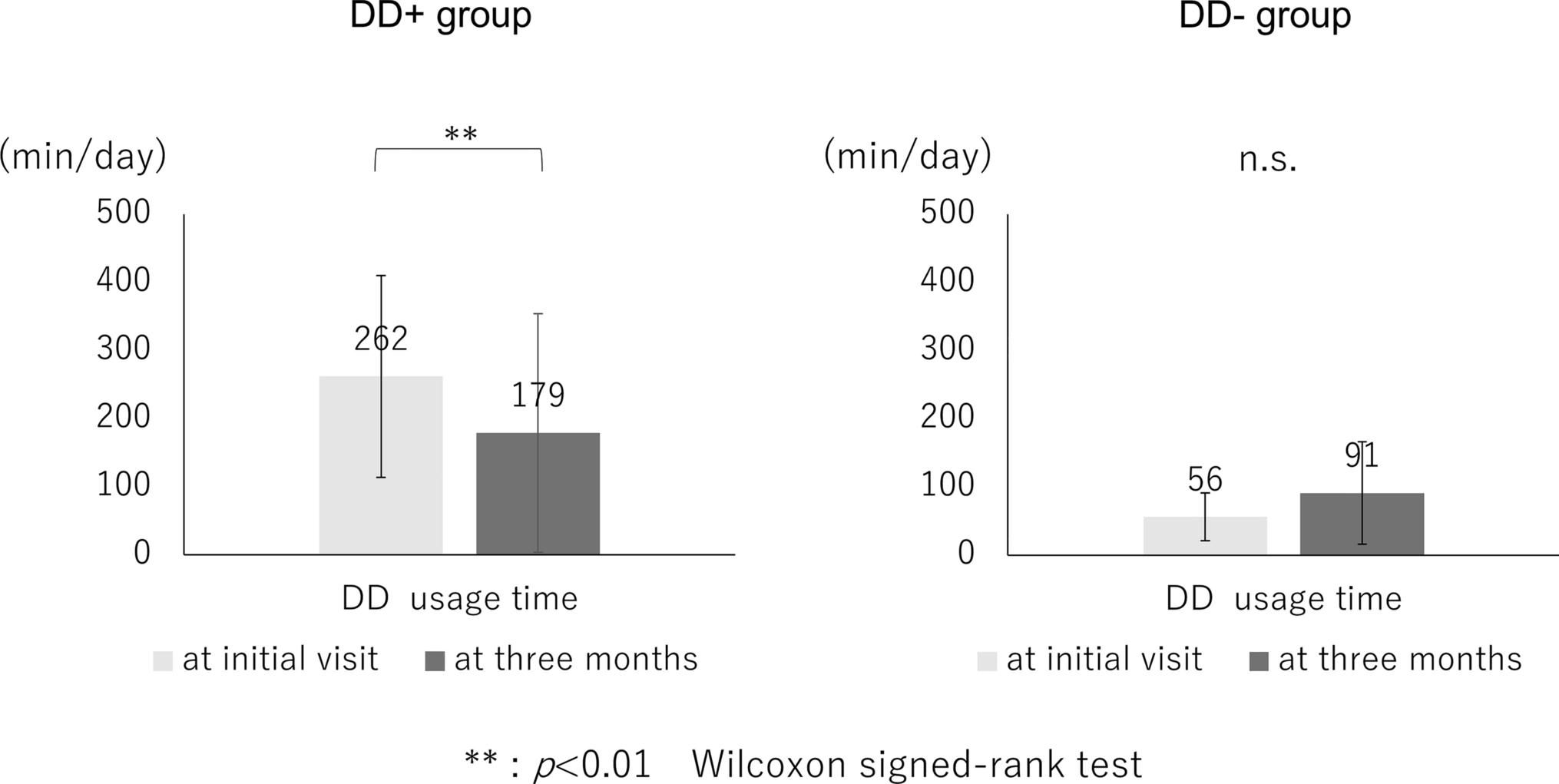
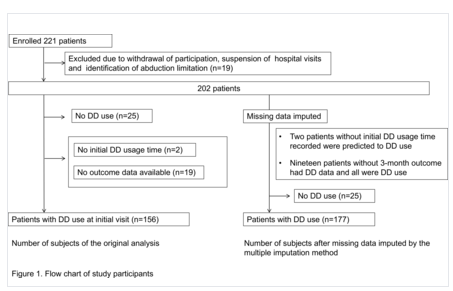
This study included subjects aged 5–35 years who developed ACE within 1 year. Subjects were divided into two groups: (i) subjects who used DD for an average of ≥120 minutes/day for junior high-school students and older and ≥60 minutes/day for primary-school students and younger (DD+); and (ii) subjects who used DD for less than that (DD-) based on the questionnaire at the study’s start. During the initial visit, glasses were prescribed when necessary; verbal instructions on DD use including time reduction and viewing-distance elongation were provided. For each group, strabismus angles at the initial visit and at 3 months were compared. Cure was defined as esophoria within 8 prism diopters without symptoms.
Results
In total, 181 cases were investigated. At baseline, strabismus angles in DD+ and DD- groups were 23±14 PD and 25±15 PD at near and 25±13 PD and 27±14 PD at distance, respectively. At 3 months, they were 22±16 PD and 25±15 PD at near and 23±14 PD and 27±13 PD at distance, respectively. Only in the DD+ group, reduction in strabismus angle was observed, but this was not clinically significant. Ten and 1 subjects in DD+ and DD- groups were cured.
Conclusion
Although changes in strabismus angles were not large enough, DD use instructions were beneficial for some ACE subjects.
デジタル機器の使用制限を伴う後天性内斜視の転帰に影響する因子: ACE-DD研究3 Factors affecting outcome of acquired comitant esotropia with restricted use of digital devices: ACEDD Study 3
Noriko Nishikawa,Hirohito Iimori,Reiko Kinouchi,Sachiko Nishina,Tomoyo Yoshida,…
BMJ Open Ophthalmol Published:31 October 2024
DOI:https://bmjophth.bmj.com/content/bmjophth/9/1/e001713.full.pdf
Abstract
Objective The objective of this study is to investigate factors associated with outcomes after 3 months of instructed usage of hand-held digital devices (DD) in patients with acquired comitant esotropia (ACE).
Methods and analysis This prospective multicentre observational study included patients with ACE, aged 5–35 years, who used DD within 1 year of onset and were followed up for clinical findings and instructed use of DD. The outcomes were classified into four groups: cured, improved, unchanged and worsened. After the analysis of group differences in the clinical and DD use-related factors by univariate analysis, we used ordinal logistic regression models to identify factors associated with favourable outcomes.
Results Of 156 patients (mean age (SD): 16.4 (7.4) years), 10 (6%), 58 (37%), 67 (43%) and 21 (14%) were classified into the cured, improved, unchanged, and worsened, respectively. In the univariate analysis, consultation within 3 months of onset, small-angle strabismus at distance and good stereoacuity were associated with good outcomes. Ordinal logistic regression analysis on adjusting for age with stereoacuity or successful DD-use time halving showed that small-angle strabismus at distance (OR: 1.02, 95% CI 1.00 to 1.03, p=0.023), good stereoacuity (OR: 1.31; 95% CI 1.10 to 1.56; p=0.003) and successful halving of DD-use time (OR: 0.63; 95% CI 0.43 to 0.92; p=0.016) influenced favourable outcomes.
Conclusion Patients with small-angle esotropia, good stereoacuity on consultation and success in halving DD-use time had a higher chance of recovery through instructional DD usage. Further studies using objectively measurable systems are needed to ensure the accuracy of DD-use time.