2026-02-16 国立循環器病研究センター
<関連情報>
- https://www.ncvc.go.jp/hospital/topics/topics_36782/
- https://www.atherosclerosis-journal.com/article/S0021-9150(26)00040-7/abstract
家族性高コレステロール血症における虚血性脳卒中および頭蓋内大動脈疾患リスク:日本における前向き研究 Ischemic stroke and intracranial large-artery disease risk in familial hypercholesterolemia: A prospective Japanese study
Yorito Hattori ∙ Kotaro Noda ∙ Mika Hori ∙ … ∙ Shuhei Yamaguchi ∙ Mariko Harada-Shiba ∙ Masafumi Ihara
Atherosclerosis Published:February 11, 2026
DOI:https://doi.org/10.1016/j.atherosclerosis.2026.120674
Highlights
- Familial hypercholesterolemia (FH) was a significant risk of intracranial large-artery disease in the Japanese population.
- FH was an independent risk for high incidence of ischemic stroke in the Japanese population.
- Intracranial large-artery disease was an independent risk factor for ischemic stroke in Japanese patients with FH.
- These findings highlight the importance of considering ethnic and genetic differences in stroke prevention strategies.
- Appropriate management of FH should be central to precision medicine approaches for reducing burden of stroke in Japan.
Abstract
Background and aims
The contribution of dyslipidemia to stroke risk is generally considered weaker than that of hypertension and diabetes. However, some previous studies suggest that dyslipidemia is associated with intracranial major artery stenosis (ICAS) and ischemic stroke, particularly in Asians populations, who are more susceptible to ICAS than Caucasians. We hypothesized that dyslipidemia, and specifically familial hypercholesterolemia (FH), may play a different role in the development of stroke in Asian populations. This study aimed to assess the prevalence and incidence of symptomatic ischemic stroke and ICAS in Japanese patients with FH compared to individuals undergoing Brain Dock.
Methods
This prospective longitudinal study included FH patients who visited a lipid clinic and underwent brain magnetic resonance imaging (MRI) at the National Cerebral and Cardiovascular Center, alongside participants who underwent brain MRI as part of the Brain Dock screening program in Japan.
Results
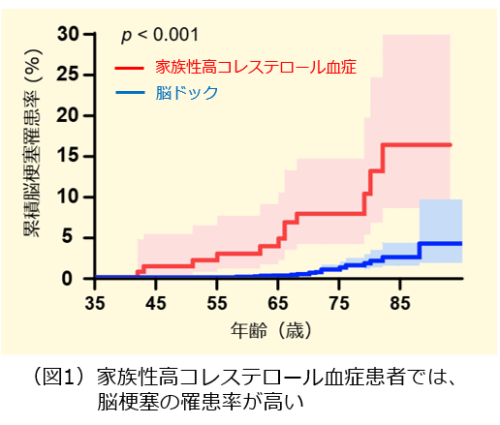
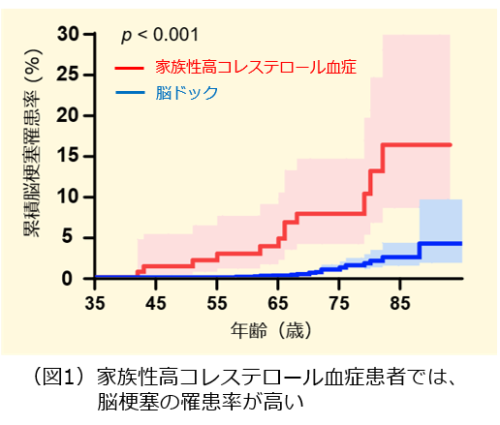
In total, 3178 participants who underwent Brain Dock and 150 patients with FH were included. FH was an independent risk factor of a higher prevalence of ICAS (≥50%; adjusted odds ratio: 17.82, 95% confidence interval [CI]: 8.74–36.36), and high symptomatic ischemic stroke incidence (adjusted hazard ratio [aHR]: 5.83, 95% CI: 2.03–16.77). The presence of ICAS was significantly associated with symptomatic ischemic stroke in patients with FH (aHR: 7.73, 95% CI: 1.53–39.06).
Conclusions
FH may confer a high risk for symptomatic ischemic stroke along with intracranial major artery changes in Japanese patients. These findings highlight the importance of considering ethnic and genetic differences in stroke prevention strategies.