国際的な分析により、2 種類の HPV 検査の結果の不一致が患者の予後を悪化させることが判明 International analysis has found that discordant results between two types of HPV test linked with worse outcomes for patients
2023-02-14 バーミンガム大学
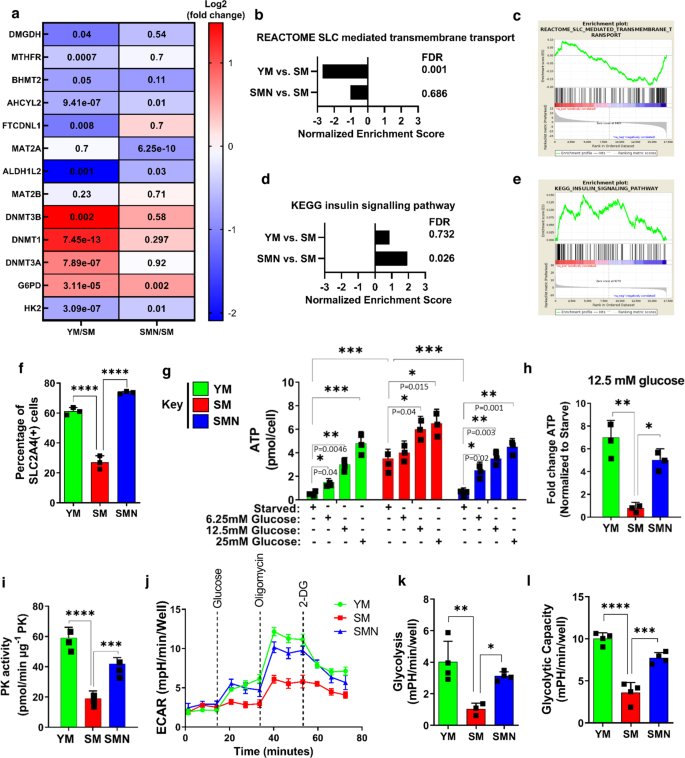
◆Lancet Oncology誌に掲載された大規模な国際試験は、世界9カ国の13の頭頸部がんセンターからの研究を調査したものである。7,895人の患者のデータから、HPVの2種類の検査で異なる結果を示す「不一致」の人が相当数いることが判明した。
◆この研究では、HPVの検査結果が不一致の患者さんの10人に1人は、両方の検査で陰性だった患者さんと比較して、治療成績が著しく悪化していることがわかりました。
◆その場合、5年全生存率は、二重陽性では81%。p16-/HPV+の患者さんでは53%。p16+/HPV-検査の患者さんでは54%。
がんがHPVに関連しているかどうかの検査は、2種類の検査で構成されています。1つ目は、HPV検査と呼ばれるもので、腫瘍の中にある実際のウイルスを調べます。もう一つは、P16というタンパク質を調べるもので、HPVのバイオマーカーとして一般的に用いられています。P16は使いやすいので、ほとんどの人がこれを標準として使っています。
<関連情報>
- https://www.birmingham.ac.uk/news/2023/conundrum-solved-over-hpv-link-with-head-and-neck-cancer
- https://www.thelancet.com/journals/lanonc/article/PIIS1470-2045(23)00013-X/fulltext
頭頸部癌におけるp16とHPVの不一致の予後への影響(HNCIG-EPIC-OPC):多施設、多国籍、個別患者データ解析 Prognostic implications of p16 and HPV discordance in oropharyngeal cancer (HNCIG-EPIC-OPC): a multicentre, multinational, individual patient data analysis
Hisham Mehanna, Miren Taberna, Christian von Buchwald, Sara Tous, Jill Brooks, Marisa Mena, Francisca Morey, Prof Christian Grønhøj, Jacob Høygaard Rasmussen, Martin Garset-Zamani, Laia Bruni, Nikolaos Batis, Ruud H Brakenhoff, C René Leemans, Robert J Baatenburg de Jong, Jens Peter Klussmann, Nora Wuerdemann,Steffen Wagner,Tina Dalianis,Linda Marklund, Haïtham Mirghani, Andrew Schache, Jaqueline A James, Shao Hui Huang, Brian O’Sullivan, Paul Nankivell, Martina A Broglie, Markus Hoffmann, Elgar Susanne Quabius, Laia Alemany, on behalf of the HNCIG-EPIC group
Lancet Oncology Published:February 13, 2023
DOI:https://doi.org/10.1016/S1470-2045(23)00013-X

Summary
Background
p16INK4a (p16) immunohistochemistry is the most widely used biomarker assay for inferring HPV causation in oropharyngeal cancer in clinical and trial settings. However, discordance exists between p16 and HPV DNA or RNA status in some patients with oropharyngeal cancer. We aimed to clearly quantify the extent of discordance, and its prognostic implications.
Methods
In this multicentre, multinational individual patient data analysis, we did a literature search in PubMed and Cochrane database for systematic reviews and original studies published in English between Jan 1, 1970, and Sept 30, 2022. We included retrospective series and prospective cohorts of consecutively recruited patients previously analysed in individual studies with minimum cohort size of 100 patients with primary squamous cell carcinoma of the oropharynx. Patient inclusion criteria were diagnosis with a primary squamous cell carcinoma of oropharyngeal cancer; data on p16 immunohistochemistry and on HPV testing; information on age, sex, tobacco, and alcohol use; staging by TNM 7th edition; information on treatments received; and data on clinical outcomes and follow-up (date of last follow-up if alive, date of recurrence or metastasis, and date and cause of death). There were no limits on age or performance status. The primary outcomes were the proportion of patients of the overall cohort who showed the different p16 and HPV result combinations, as well as 5-year overall survival and 5-year disease-free survival. Patients with recurrent or metastatic disease or who were treated palliatively were excluded from overall survival and disease-free survival analyses. Multivariable analysis models were used to calculate adjusted hazard ratios (aHR) for different p16 and HPV testing methods for overall survival, adjusted for prespecified confounding factors.
Findings
Our search returned 13 eligible studies that provided individual data for 13 cohorts of patients with oropharyngeal cancer from the UK, Canada, Denmark, Sweden, France, Germany, the Netherlands, Switzerland, and Spain. 7895 patients with oropharyngeal cancer were assessed for eligibility. 241 were excluded before analysis, and 7654 were eligible for p16 and HPV analysis. 5714 (74·7%) of 7654 patients were male and 1940 (25·3%) were female. Ethnicity data were not reported. 3805 patients were p16-positive, 415 (10·9%) of whom were HPV-negative. This proportion differed significantly by geographical region and was highest in the areas with lowest HPV-attributable fractions (r=–0·744, p=0·0035). The proportion of patients with p16+/HPV– oropharyngeal cancer was highest in subsites outside the tonsil and base of tongue (29·7% vs 9·0%, p<0·0001). 5-year overall survival was 81·1% (95% CI 79·5–82·7) for p16+/HPV+, 40·4% (38·6–42·4) for p16–/HPV–, 53·2% (46·6–60·8) for p16–/HPV+, and 54·7% (49·2–60·9) for p16+/HPV–. 5-year disease-free survival was 84·3% (95% CI 82·9–85·7) for p16+/HPV+, 60·8% (58·8–62·9) for p16–/HPV–; 71·1% (64·7–78·2) for p16–/HPV+, and 67·9% (62·5–73·7) for p16+/HPV–. Results were similar across all European sub-regions, but there were insufficient numbers of discordant patients from North America to draw conclusions in this cohort.
Interpretation
Patients with discordant oropharyngeal cancer (p16–/HPV+ or p16+/HPV–) had a significantly worse prognosis than patients with p16+/HPV+ oropharyngeal cancer, and a significantly better prognosis than patients with p16–/HPV– oropharyngeal cancer. Along with routine p16 immunohistochemistry, HPV testing should be mandated for clinical trials for all patients (or at least following a positive p16 test), and is recommended where HPV status might influence patient care, especially in areas with low HPV-attributable fractions.
Funding
European Regional Development Fund, Generalitat de Catalunya, National Institute for Health Research (NIHR) UK, Cancer Research UK, Medical Research Council UK, and The Swedish Cancer Foundation and the Stockholm Cancer Society.