2024-10-23 ワシントン大学セントルイス校
<関連情報>
- https://source.washu.edu/2024/10/immunotherapy-blocks-scarring-improves-heart-function-in-mice-with-heart-failure/
- https://www.nature.com/articles/s41586-024-08008-5
心不全における免疫-線維芽細胞コミュニケーションを標的とする Targeting immune–fibroblast cell communication in heart failure
Junedh M. Amrute,Xin Luo,Vinay Penna,Steven Yang,Tracy Yamawaki,Sikander Hayat,Andrea Bredemeyer,In-Hyuk Jung,Farid F. Kadyrov,Gyu Seong Heo,Rajiu Venkatesan,Sally Yu Shi,Alekhya Parvathaneni,Andrew L. Koenig,Christoph Kuppe,Candice Baker,Hannah Luehmann,Cameran Jones,Benjamin Kopecky,Xue Zeng,Tore Bleckwehl,Pan Ma,Paul Lee,Yuriko Terada,… Kory J. Lavine
Nature Published:23 October 2024
DOI:https://doi.org/10.1038/s41586-024-08008-5
Abstract
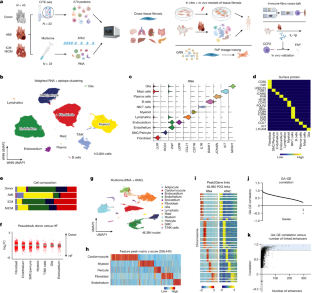
Inflammation and tissue fibrosis co-exist and are causally linked to organ dysfunction1,2. However, the molecular mechanisms driving immune–fibroblast cell communication in human cardiac disease remain unexplored and there are at present no approved treatments that directly target cardiac fibrosis3,4. Here we performed multiomic single-cell gene expression, epitope mapping and chromatin accessibility profiling in 45 healthy donor, acutely infarcted and chronically failing human hearts. We identified a disease-associated fibroblast trajectory that diverged into distinct populations reminiscent of myofibroblasts and matrifibrocytes, the latter expressing fibroblast activator protein (FAP) and periostin (POSTN). Genetic lineage tracing of FAP+ fibroblasts in vivo showed that they contribute to the POSTN lineage but not the myofibroblast lineage. We assessed the applicability of experimental systems to model cardiac fibroblasts and demonstrated that three different in vivo mouse models of cardiac injury were superior compared with cultured human heart and dermal fibroblasts in recapitulating the human disease phenotype. Ligand–receptor analysis and spatial transcriptomics predicted that interactions between C-C chemokine receptor type 2 (CCR2) macrophages and fibroblasts mediated by interleukin-1β (IL-1β) signalling drove the emergence of FAP/POSTN fibroblasts within spatially defined niches. In vivo, we deleted the IL-1 receptor on fibroblasts and the IL-1β ligand in CCR2+ monocytes and macrophages, and inhibited IL-1β signalling using a monoclonal antibody, and showed reduced FAP/POSTN fibroblasts, diminished myocardial fibrosis and improved cardiac function. These findings highlight the broader therapeutic potential of targeting inflammation to treat tissue fibrosis and preserve organ function.