2025-07-02 バース大学
<関連情報>
- https://www.bath.ac.uk/announcements/too-many-medicines-too-many-hospital-visits-new-study-highlights-hidden-risk-for-older-adults/
- https://academic.oup.com/ageing/article/54/6/afaf156/8158005
- https://academic.oup.com/biomedgerontology/article/79/8/glae130/7668504
潜在的に不適切なポリファーマシーは高齢者の30日緊急入院の重要な予測因子である:機械学習による特徴検証研究 Potentially inappropriate polypharmacy is an important predictor of 30-day emergency hospitalisation in older adults: a machine learning feature validation study
Robert T Olender , Sandipan Roy , Prasad S Nishtala
Age and Ageing Published:06 June 2025
DOI:https://doi.org/10.1093/ageing/afaf156
Abstract
Background
Machine learning (ML) models in healthcare are crucial for predicting clinical outcomes, and their effectiveness can be significantly enhanced through improvements in accuracy, generalisability, and interpretability. To achieve widespread adoption in clinical practice, risk factors identified by these models must be validated in diverse populations.
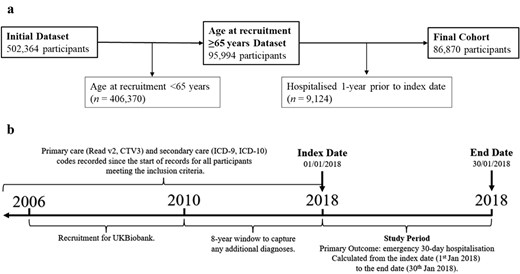
Methods
In this cohort study, 86 870 community-dwelling older adults ≥65 years from the UK Biobank database were used to train and test three ML models to predict 30-day emergency hospitalisation. The three ML models, Random Forest (RF), XGBoost (XGB), and Logistic Regression (LR), utilised all extracted variables, consisting of demographic and geriatric syndromes, comorbidities, and the Drug Burden Index (DBI), a measure of potentially inappropriate polypharmacy, which quantifies exposure to medications with anticholinergic and sedative properties. 30-day emergency hospitalisation was defined as any hospitalisation related to any clinical event within 30 days of the index date. The model performance metrics included the area under the receiver operating characteristics curve (AUC-ROC) and the F1 score.
Results
The AUC-ROC for the RF, XGB and LR models was 0.78, 0.86 and 0.61, respectively, signifying good discriminatory power. The DBI, mobility, fractures, falls, hazardous alcohol drinking and smoking were validated as important variables in predicting 30-day emergency hospitalisation.
Conclusions
This study validated important risk factors for predicting 30-day emergency hospitalisation. The validation of important risk factors will inform the development of future ML studies in geriatrics. Future research should prioritise the development of targeted interventions to address the risk factors validated in this study, ultimately improving patient outcomes and alleviating healthcare burdens.
薬物負担指数は、複雑なケアを必要とする地域在住高齢者における30日入院の修正可能な予測因子である: InterRAIデータの機械学習分析 Drug Burden Index Is a Modifiable Predictor of 30-Day Hospitalization in Community-Dwelling Older Adults With Complex Care Needs: Machine Learning Analysis of InterRAI Data
Robert T Olender, MRes , Sandipan Roy, PhD , Hamish A Jamieson, PhD , Sarah N Hilmer, PhD , Prasad S Nishtala, PhD
The Journals of Gerontology: Series A Published:11 May 2024
DOI:https://doi.org/10.1093/gerona/glae130
Abstract
Background
Older adults (≥65 years) account for a disproportionately high proportion of hospitalization and in-hospital mortality, some of which may be avoidable. Although machine learning (ML) models have already been built and validated for predicting hospitalization and mortality, there remains a significant need to optimize ML models further. Accurately predicting hospitalization may tremendously affect the clinical care of older adults as preventative measures can be implemented to improve clinical outcomes for the patient.
Methods
In this retrospective cohort study, a data set of 14 198 community-dwelling older adults (≥65 years) with complex care needs from the International Resident Assessment Instrument-Home Care database was used to develop and optimize 3 ML models to predict 30-day hospitalization. The models developed and optimized were Random Forest (RF), XGBoost (XGB), and Logistic Regression (LR). Variable importance plots were generated for all 3 models to identify key predictors of 30-day hospitalization.
Results
The area under the receiver-operating characteristics curve for the RF, XGB, and LR models were 0.97, 0.90, and 0.72, respectively. Variable importance plots identified the Drug Burden Index and alcohol consumption as important, immediately potentially modifiable variables in predicting 30-day hospitalization.
Conclusions
Identifying immediately potentially modifiable risk factors such as the Drug Burden Index and alcohol consumption is of high clinical relevance. If clinicians can influence these variables, they could proactively lower the risk of 30-day hospitalization. ML holds promise to improve the clinical care of older adults. It is crucial that these models undergo extensive validation through large-scale clinical studies before being utilized in the clinical setting.


