2025-09-08 バッファロー大学 (UB)
<関連情報>
- https://www.buffalo.edu/news/releases/2025/09/Oral-Mucositis-AI-prediction-tool.html
- https://www.mdpi.com/2072-6694/17/16/2657
- https://link.springer.com/article/10.1007/s00520-025-09691-4
造血幹細胞移植後の口腔粘膜炎に関連する感染性合併症の発生リスク上昇:転帰と危険因子に関する系統的レビューとメタ分析 Elevated Likelihood of Infectious Complications Related to Oral Mucositis After Hematopoietic Stem Cell Transplantation: A Systematic Review and Meta-Analysis of Outcomes and Risk Factors
Susan Eichhorn,Lauryn Rudin,Chidambaram Ramasamy,Ridham Varsani,Parikshit Padhi,Nour Nassour,Kapil Meleveedu,Joel B. Epstein,Benjamin Semegran,Roberto Pili and Poolakkad S. Satheeshkumar
Cancers Published: 14 August 2025
DOI:https://doi.org/10.3390/cancers17162657
Simple Summary
Oral mucositis (OM) is a frequent, debilitating side effect of hematopoietic stem cell transplantation (HSCT), significantly impacting patient outcomes and quality of life. This systematic review and meta-analysis attempted to establish risk factors for OM and its association with infectious complications in recipients of HSCT. Thirty-four studies were conducted, and high-intensity conditioning, administration of methotrexate, female sex, longer neutropenia/neutrophil engraftment, reactivation of HSV-1 infection, and renal impairment appeared as significant risk factors for OM. This meta-analysis demonstrated that patients suffering from OM had nearly four times the risk of developing infections compared with non-OM patients. These findings indicate the importance of early OM diagnosis and OM-prevention strategies in restricting severe complications in immunocompromised patients receiving HSCT.
Abstract
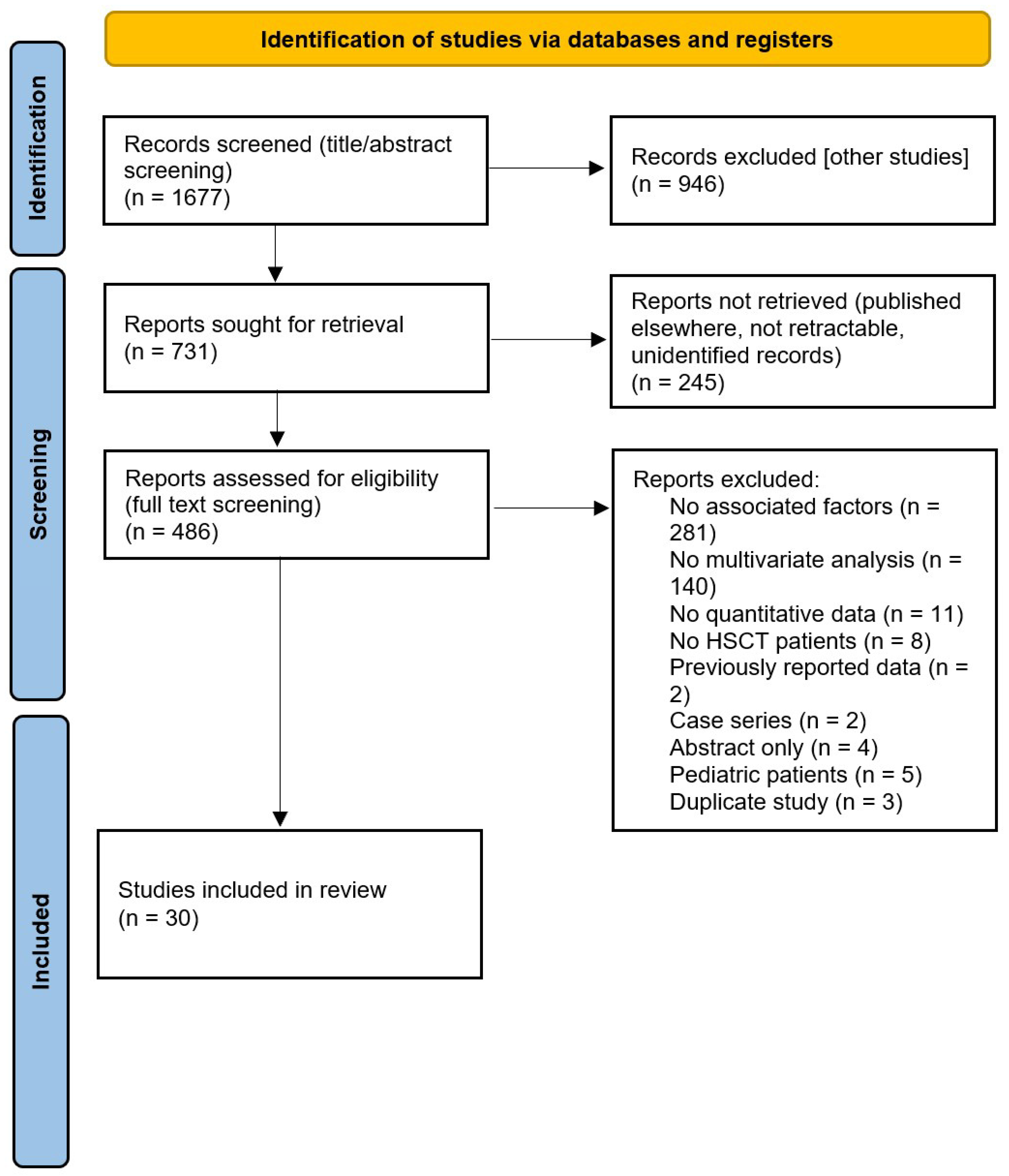
Mucositis involving the gastrointestinal, vaginal, and nasal mucosa is one of the primary dose-limiting toxicities of hematopoietic stem cell transplantation (HSCT) and its conditioning regimen. The oropharyngeal mucosa is commonly affected, which can be detrimental to patient health and quality of life. Despite its significant prevalence and deleterious effects, we have an inadequate understanding of the risk factors and outcomes associated with oral mucositis (OM). We performed a literature search through PubMed and EBSCO (inception to 31 March 2024) following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Data was extracted from eligible studies using a pre-specified data extraction form. Quality of the data was assessed using the Newcastle-Ottawa Scale for non-randomized, observational studies and the Cochrane Collaboration Tool for randomized controlled trials. Our initial search identified 1677 articles, 34 of which were included in our study. Of those 34, 30 were included in the qualitative assessment of clinical risk factors in the development of OM, and 4 were included in the meta-analysis assessing the relationship between OM and infectious complications following HSCT. Across both HSCT modalities and cancer cohorts, female sex and high-intensity conditioning were common risk factors in the development of OM. When stratified by allogeneic and autologous HSCT, methotrexate, younger age, and longer duration of neutropenia were associated with increased OM risk in allogeneic HSCT recipients, while renal dysfunction, HSV-1 reactivation, and longer neutrophil engraftment were associated with increased OM risk in autologous HSCT recipients. Longer neutrophil engraftment was a common risk factor across different cancer cohorts; however, renal dysfunction was a distinct risk factor for OM in multiple myeloma patients. Additionally, our meta-analysis revealed that patients with OM have an increased risk of developing infectious complications following HSCT compared to those without OM, with an odds ratio of 3.84 (95% CI: 2.51–5.86). The development of OM is related to various risk factors, and individuals with OM are at greater risk of infectious complications. Knowledge of these risk factors and outcomes will help clinicians identify high-risk individuals, prevent OM, and protect an immunocompromised population from subsequent life-threatening complications.
がん治療誘発性毒性の予測が支持療法の指針となる可能性―重度口腔粘膜炎予測のためのノモグラム活用に関する方法論論文、第1部 Guided supportive care may benefit from predicting cancer treatment-induced toxicity—a methodology paper on utilization of nomograms to predict severe oral mucositis, Part I
Poolakkad S. Satheeshkumar,Joel B. Epstein,Deepshikha Kewlani & Roberto Pili
Supportive Care in Cancer Published:01 July 2025
DOI:https://doi.org/10.1007/s00520-025-09691-4
Abstract
Background
Patients undergoing hematopoietic stem cell transplantation (HSCT) should maintain oral hygiene to minimize mouth problems from the high-dose conditioning regimen. Utilizing risk prediction tools such as nomograms may be beneficial in predicting severe oral complications such as mucositis.
Methods
A study was performed using the National Inpatient Samples Database 2018 to investigate individuals admitted to the hospital for autologous HSCT. The nomogram tool was employed to predict oral ulcerative mucositis (UM), utilizing a logistic regression model with the variables age, gender, race, total body irradiation (TBI), and fluid and electrolyte disorders (fed), and further we applied our findings in 2021 autologous HSCT cohorts and 2018 allogenic HSCT cohorts.
Results
A total of 1560 patients who encountered UM were identified among 10,700 patients who underwent HSCT. The analysis showed that a 30-year-old White female patient who undergoes HSCT has a 28.2% risk of developing UM, 95%CI: 17.1–42.9%, who also undertook TBI, and had fed. On the other hand, a 20-year-old White female patient who undergoes HSCT has a risk score of 28.9% (95%CI: 17.6–46.0%), who also underwent TBI, and had fed. Additionally, Black female patient with TBI and fed of the same age of 20 or 30 who undergoes HSCT along with TBI has a risk score of 29.3% (95%CI: 17.3–45.1%), and 27.7%; 95%CI: 16.8–42.0%. The application in 2021 and 2018 cohorts showed similar trends, UM risk higher in allogenic cohorts with 47.2% risk (95%CI: 37.7–57.09%) in a White female, having weight loss and TBI.
Conclusion
This report shows that younger age group, females, Whites, and those who are expected to receive TBI and having fed could be considered to be at a higher risk for developing severe mucositis. Thus, routine use of nomogram can help identify those requiring enhanced preventive oral care for reducing the oral complications such as UM.