前頭側頭型認知症では、統合失調症と同じ脳内ネットワークが影響を受ける可能性がある In frontotemporal dementia, the same brain networks can be affected as in schizophrenia
2022-08-04 マックス・プランク研究所


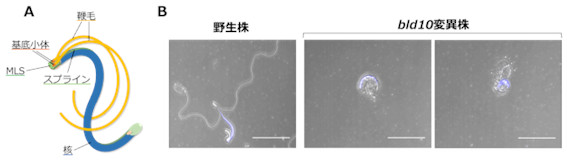
Neuroanatomical patterns of the behavioral variant of frontotemporal dementia (top) and schizophrenia
前頭側頭型認知症(FTD)、特に行動バリアント (bvFTD) は、統合失調症と混同されることが多いため、初期の段階で気づくのは困難です。
人工知能を用いて両疾患の神経解剖学的分類法を訓練し、それを異なるコホートの脳データに対して適用した。その結果、統合失調症患者の41%がbvFTDの基準を満たしたことが、権威あるJAMA Psychiatry誌に発表されました。
研究チームは、2つの疾患の類似性を示すbvFTDスコアが高い患者ほど、「bvFTD様」の表現型を持ち、2年間で症状が改善する可能性が低いことを発見しました。
bvFTDでは、特定のニューロン(von Economoニューロン)が滅失します。統合失調症では、これらのニューロンにも変化が見られます。
<関連情報>
- https://www.mpg.de/19060423/0804-pskl-schizophrenie-und-demenz-153150-x
- https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2794930
多峰性機械学習による精神病と前頭側頭型認知症の関連性の探索 前駆病変の再考 Exploring Links Between Psychosis and Frontotemporal Dementia Using Multimodal Machine Learning Dementia Praecox Revisited
Nikolaos Koutsouleris, Christos Pantelis, Dennis Velakoulis, Philip McGuire, Dominic B. Dwyer,Maria-Fernanda Urquijo-Castro, Riya Paul, Sen Dong, David Popovic, Oemer Oeztuerk, Joseph Kambeitz, Raimo K. R. Salokangas, Jarmo Hietala, Alessandro Bertolino,Paolo Brambilla, Rachel Upthegrove, Stephen J. Wood, Rebekka Lencer, Stefan Borgwardt, Carlo Maj, Markus Nöthen,Franziska Degenhardt, Maryna Polyakova, Karsten Mueller, Arno Villringer, Adrian Danek, Klaus Fassbender,Klaus Fliessbach,Holger Jahn, Johannes Kornhuber, Bernhard Landwehrmeyer,Sarah Anderl-Straub, Johannes Prudlo, Matthis Synofzik, Jens Wiltfang, Lina Riedl, Janine Diehl-Schmid,Markus Otto, Eva Meisenzahl, Peter Falkai, Matthias L. Schroeter,
JAMA Psychiatry Published:August 3, 2022
DOI:10.1001/jamapsychiatry.2022.2075
Key Points
Question Do psychosis and dementia share brain-behavioral alterations?
Findings In this diagnostic/prognostic study including 1870 patients, patients with schizophrenia expressed the neuroanatomical pattern of behavioral-variant frontotemporal dementia more strongly (41%) than that of Alzheimer disease (17%), and at lower levels, this difference was also encountered in those with major depression (22% vs 3%). Already in clinical high-risk states for psychosis the high expression of the behavioral-variant frontotemporal dementia pattern was linked to severe phenotypes, unfavorable courses, and elevated polygenic risks for schizophrenia and dementia, with further pattern progression being present in those patients who did not recover over time.
Meaning Dementia praecox should be revisited as a shared pathophysiological dimension of severe psychosis and frontotemporal disease spectra.
Abstract
Importance The behavioral and cognitive symptoms of severe psychotic disorders overlap with those seen in dementia. However, shared brain alterations remain disputed, and their relevance for patients in at-risk disease stages has not been explored so far.
Objective To use machine learning to compare the expression of structural magnetic resonance imaging (MRI) patterns of behavioral-variant frontotemporal dementia (bvFTD), Alzheimer disease (AD), and schizophrenia; estimate predictability in patients with bvFTD and schizophrenia based on sociodemographic, clinical, and biological data; and examine prognostic value, genetic underpinnings, and progression in patients with clinical high-risk (CHR) states for psychosis or recent-onset depression (ROD).
Design, Setting, and Participants This study included 1870 individuals from 5 cohorts, including (1) patients with bvFTD (n = 108), established AD (n = 44), mild cognitive impairment or early-stage AD (n = 96), schizophrenia (n = 157), or major depression (n = 102) to derive and compare diagnostic patterns and (2) patients with CHR (n = 160) or ROD (n = 161) to test patterns’ prognostic relevance and progression. Healthy individuals (n = 1042) were used for age-related and cohort-related data calibration. Data were collected from January 1996 to July 2019 and analyzed between April 2020 and April 2022.
Main Outcomes and Measures Case assignments based on diagnostic patterns; sociodemographic, clinical, and biological data; 2-year functional outcomes and genetic separability of patients with CHR and ROD with high vs low pattern expression; and pattern progression from baseline to follow-up MRI scans in patients with nonrecovery vs preserved recovery.
Results Of 1870 included patients, 902 (48.2%) were female, and the mean (SD) age was 38.0 (19.3) years. The bvFTD pattern comprising prefrontal, insular, and limbic volume reductions was more expressed in patients with schizophrenia (65 of 157 [41.2%]) and major depression (22 of 102 [21.6%]) than the temporo-limbic AD patterns (28 of 157 [17.8%] and 3 of 102 [2.9%], respectively). bvFTD expression was predicted by high body mass index, psychomotor slowing, affective disinhibition, and paranoid ideation (R2 = 0.11). The schizophrenia pattern was expressed in 92 of 108 patients (85.5%) with bvFTD and was linked to the C9orf72 variant, oligoclonal banding in the cerebrospinal fluid, cognitive impairment, and younger age (R2 = 0.29). bvFTD and schizophrenia pattern expressions forecasted 2-year psychosocial impairments in patients with CHR and were predicted by polygenic risk scores for frontotemporal dementia, AD, and schizophrenia. Findings were not associated with AD or accelerated brain aging. Finally, 1-year bvFTD/schizophrenia pattern progression distinguished patients with nonrecovery from those with preserved recovery.
Conclusions and Relevance Neurobiological links may exist between bvFTD and psychosis focusing on prefrontal and salience system alterations. Further transdiagnostic investigations are needed to identify shared pathophysiological processes underlying the neuroanatomical interface between the 2 disease spectra.