2024-03-07 インペリアル・カレッジ・ロンドン(ICL)
<関連情報>
- https://www.imperial.ac.uk/news/251878/could-dna-diet-help-reduce-health/
- https://www.nature.com/articles/s41598-024-55105-6%C2%A0
26週間にわたるグルコース調節障害における個別化栄養介入の影響評価:無作為化比較試験 Assessment of the impact of a personalised nutrition intervention in impaired glucose regulation over 26 weeks: a randomised controlled trial
Maria Karvela,Caroline T. Golden,Nikeysha Bell,Stephanie Martin-Li,Judith Bedzo-Nutakor,Natalie Bosnic,Pierre DeBeaudrap,Sara de Mateo-Lopez,Ahmed Alajrami,Yun Qin,Maria Eze,Tsz-Kin Hon,Javier Simón-Sánchez,Rashmita Sahoo,Jonathan Pearson-Stuttard,Patrick Soon-Shiong,Christofer Toumazou & Nick Oliver
Scientific Reports Published:05 March 2024
DOI:https://doi.org/10.1038/s41598-024-55105-6
Abstract
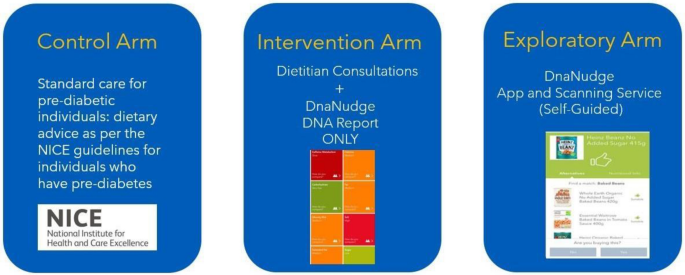
Dietary interventions can reduce progression to type 2 diabetes mellitus (T2DM) in people with non-diabetic hyperglycaemia. In this study we aimed to determine the impact of a DNA-personalised nutrition intervention in people with non-diabetic hyperglycaemia over 26 weeks. ASPIRE-DNA was a pilot study. Participants were randomised into three arms to receive either (i) Control arm: standard care (NICE guidelines) (n = 51), (ii) Intervention arm: DNA-personalised dietary advice (n = 50), or (iii) Exploratory arm: DNA-personalised dietary advice via a self-guided app and wearable device (n = 46). The primary outcome was the difference in fasting plasma glucose (FPG) between the Control and Intervention arms after 6 weeks. 180 people were recruited, of whom 148 people were randomised, mean age of 59 years (SD = 11), 69% of whom were female. There was no significant difference in the FPG change between the Control and Intervention arms at 6 weeks (- 0.13 mmol/L (95% CI [- 0.37, 0.11]), p = 0.29), however, we found that a DNA-personalised dietary intervention led to a significant reduction of FPG at 26 weeks in the Intervention arm when compared to standard care (- 0.019 (SD = 0.008), p = 0.01), as did the Exploratory arm (- 0.021 (SD = 0.008), p = 0.006). HbA1c at 26 weeks was significantly reduced in the Intervention arm when compared to standard care (- 0.038 (SD = 0.018), p = 0.04). There was some evidence suggesting prevention of progression to T2DM across the groups that received a DNA-based intervention (p = 0.06). Personalisation of dietary advice based on DNA did not result in glucose changes within the first 6 weeks but was associated with significant reduction of FPG and HbA1c at 26 weeks when compared to standard care. The DNA-based diet was effective regardless of intervention type, though results should be interpreted with caution due to the low sample size. These findings suggest that DNA-based dietary guidance is an effective intervention compared to standard care, but there is still a minimum timeframe of adherence to the intervention before changes in clinical outcomes become apparent.


