2024-1-18 マサチューセッツ大学アマースト校
◆この発見から、結核治療において免疫反応全体を対象とする総合的なアプローチが有効である可能性が示唆されており、これが新しい治療戦略につながる可能性がある。
<関連情報>
- https://www.umass.edu/news/article/remodeling-immune-system-fight-tuberculosis
- https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1011871
- https://www.science.org/doi/full/10.1126/sciimmunol.aaw6693
結核菌への曝露は肺胞マクロファージと結核菌感染に対する初期自然応答をリモデリングする Exposure to Mycobacterium remodels alveolar macrophages and the early innate response to Mycobacterium tuberculosis infection
Dat Mai,Ana Jahn,Tara Murray,Michael Morikubo,Pamelia N. Lim,Maritza M. Cervantes,Linh K. Pham,Johannes Nemeth,Kevin Urdahl,Alan H. Diercks,Alan Aderem,Alissa C. Rothchild
PLOS Pathogens Published: January 18, 2024
DOI:https://doi.org/10.1371/journal.ppat.1011871
Abstract
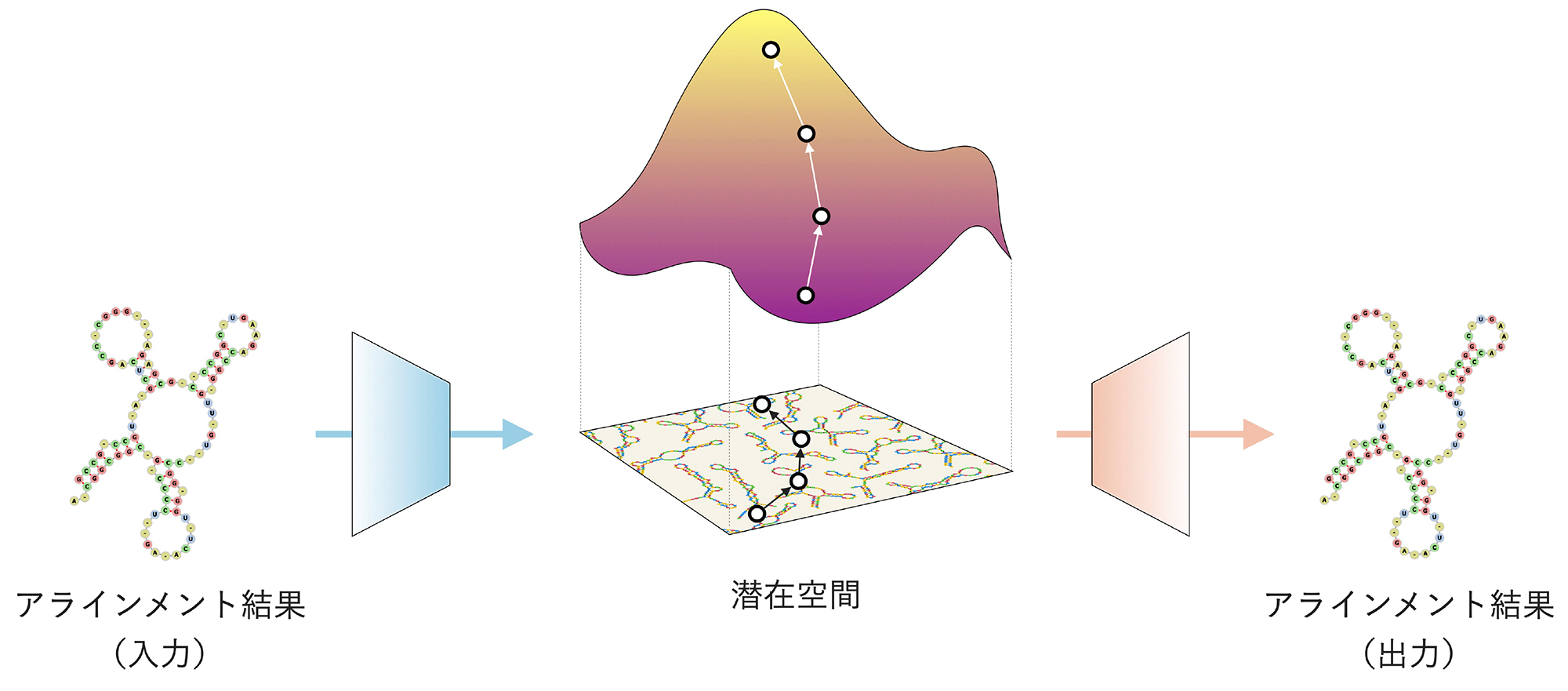
Alveolar macrophages (AMs) play a critical role during Mycobacterium tuberculosis (Mtb) infection as the first cells in the lung to encounter bacteria. We previously showed that AMs initially respond to Mtb in vivo by mounting a cell-protective, rather than pro-inflammatory response. However, the plasticity of the initial AM response was unknown. Here, we characterize how previous exposure to Mycobacterium, either through subcutaneous vaccination with Mycobacterium bovis (scBCG) or through a contained Mtb infection (coMtb) that mimics aspects of concomitant immunity, impacts the initial response by AMs. We find that both scBCG and coMtb accelerate early innate cell activation and recruitment and generate a stronger pro-inflammatory response to Mtb in vivo by AMs. Within the lung environment, AMs from scBCG vaccinated mice mount a robust interferon-associated response, while AMs from coMtb mice produce a broader inflammatory response that is not dominated by Interferon Stimulated Genes. Using scRNAseq, we identify changes to the frequency and phenotype of airway-resident macrophages following Mycobacterium exposure, with enrichment for both interferon-associated and pro-inflammatory populations of AMs. In contrast, minimal changes were found for airway-resident T cells and dendritic cells after exposures. Ex vivo stimulation of AMs with Pam3Cys, LPS and Mtb reveal that scBCG and coMtb exposures generate stronger interferon-associated responses to LPS and Mtb that are cell-intrinsic changes. However, AM profiles that were unique to each exposure modality following Mtb infection in vivo are dependent on the lung environment and do not emerge following ex vivo stimulation. Overall, our studies reveal significant and durable remodeling of AMs following exposure to Mycobacterium, with evidence for both AM-intrinsic changes and contributions from the altered lung microenvironments. Comparisons between the scBCG and coMtb models highlight the plasticity of AMs in the airway and opportunities to target their function through vaccination or host-directed therapies.
Author summary
Tuberculosis, a disease caused by the bacteria Mycobacterium tuberculosis (Mtb), claims around 1.6 million lives each year, making it one of the leading causes of death worldwide by an infectious agent. Based on principles of conventional immunological memory, prior exposure to either Mtb or M. bovis BCG leads to antigen-specific long-lasting changes to the adaptive immune response that can be effective at protecting against subsequent challenge. However, how these exposures may also impact the innate immune response is less understood. Alveolar macrophages are tissue-resident myeloid cells that play an important role during Mtb infection as innate immune sentinels in the lung and the first host cells to respond to infection. Here, we examined how prior Mycobacterium exposure, either through BCG vaccination or a model of contained Mtb infection, impacts the early innate response by alveolar macrophages. We find that prior exposure remodels the alveolar macrophage response to Mtb through both cell-intrinsic changes and signals that depend on the altered lung environment. These findings suggest that the early innate immune response could be targeted through vaccination or host-directed therapy and could complement existing strategies to enhance the host response to Mtb.
肺胞マクロファージはin vivoで結核菌に対して非正規NRF2駆動の転写応答を生じる Alveolar macrophages generate a noncanonical NRF2-driven transcriptional response to Mycobacterium tuberculosis in vivo
ALISSA C. ROTHCHILD , GREGORY S. OLSON , JOHANNES NEMETH , LYNN M. AMON , […], AND ALAN ADEREM
Science Immunology Published:5 Jul 2019
DOI:https://doi.org/10.1126/sciimmunol.aaw6693

Interfering with macrophage activation
One of the many reasons for Mycobacterium tuberculosis (M.tb.) persistence is that the bacterium blocks activation of M.tb.-specific immune responses. Here, using a mouse model of tuberculosis, Rothchild et al. demonstrate that M.tb.-infected alveolar macrophages in the lung show an impaired ability to drive antibacterial responses. These M.tb.-infected macrophages up-regulate an antioxidant transcription signature that is driven by the transcription factor nuclear factor erythroid 2–related factor 2 (NRF2). By infecting mice engineered to lack NRF2 in myeloid cells with M.tb., they show that loss of NRF2 in myeloid cells lowered bacterial burdens. Their studies have brought to the fore the importance of NRF2 in regulating early interactions between M.tb. and host immune cells.
Abstract
Alveolar macrophages (AMs) are the first cells to be infected during Mycobacterium tuberculosis (M.tb.) infection. Thus, the AM response to infection is the first of many steps leading to initiation of the adaptive immune response required for efficient control of infection. A hallmark of M.tb. infection is the slow initiation of the adaptive response, yet the mechanisms responsible for this are largely unknown. To study the initial AM response to infection, we developed a system to identify, sort, and analyze M.tb.-infected AMs from the lung within the first 10 days of infection. In contrast to what has been previously described using in vitro systems, M.tb.-infected AMs up-regulate a cell-protective antioxidant transcriptional signature that is dependent on the lung environment but not bacterial virulence. Computational approaches including pathway analysis and transcription factor motif enrichment analysis identify NRF2 as a master regulator of the response. Using knockout mouse models, we demonstrate that NRF2 drives expression of the cell-protective signature in AMs and impairs the control of early bacterial growth. AMs up-regulate a substantial pro-inflammatory response to M.tb. infection only 10 days after infection, yet comparisons with bystander AMs from the same infected animals demonstrate that M.tb.-infected AMs generate a less robust inflammatory response than the uninfected cells around them. Our findings demonstrate that the initial macrophage response to M.tb. in the lung is far less inflammatory than has previously been described by in vitro systems and may impede the overall host response to infection.